- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
January 31, 2017

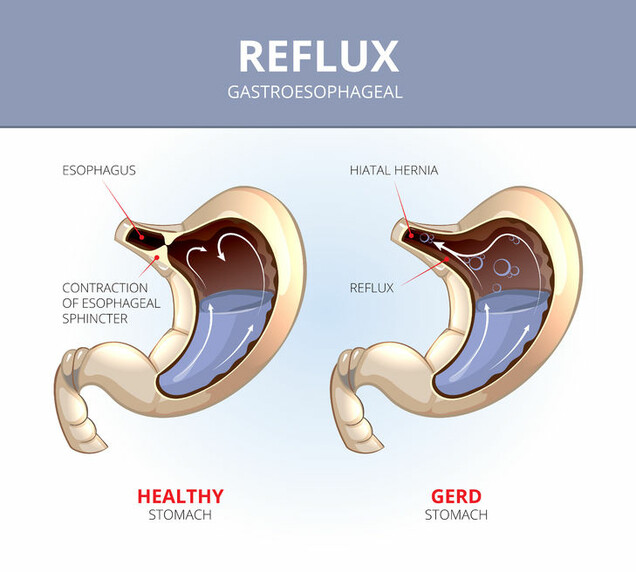
Gastroesophageal reflux disease (GERD) is a chronic digestive disease affecting the upper portion of the digestive tract. The upper digestive tract is made up of the esophagus, which is a tube of muscle that carries the food from the mouth and throat to the stomach. Gastroesophageal reflux occurs when acid or food from the stomach flows back up into the esophagus. In normal digestion, the lower esophageal sphincter (LES), which is formed by the diaphragm muscles, pinches shut the bottom part of the esophagus, preventing food and acid from the stomach from flowing back into the esophagus. When you eat or drink, the LES opens to allow food and liquid to pass into the stomach. When the LES is weak or if a hiatal hernia is present, you may experience GERD symptoms. A hiatal hernia is when a portion of the upper part of the stomach has moved up into the chest through an opening in the diaphragm muscle.
GERD is the most common digestive tract disease diagnosed during outpatient visits in the United States. It is estimated that up to 20% of Americans experience at least weekly symptoms related to GERD.
The most common symptom of GERD is a burning sensation in your chest, which many people describe as “heartburn.” Sometimes the burning sensation spreads to your throat and is accompanied by a sour or bitter taste in your mouth. The burning sensation or pain associated with heartburn can last for several hours and is often worse after eating. Bending over or lying down can also make the symptoms worse and some people are often awakened from sleep with heartburn symptoms.
The severity of GERD symptoms is a spectrum. A gastroenterologist may recommend an upper endoscopy to evaluate the esophagus. An upper endoscopy is a procedure where a flexible tube with a camera and a light is placed into the esophagus and stomach to evaluate any damage to the inside lining of the esophagus as a result of long-term reflux. In more severe cases, chronic irritation of the esophagus lining is found, sometimes with ulcers in the wall of the esophagus being identified. In some patients with severe GERD that has been untreated for a long period of time, the lining of the esophagus may have changed in response to chronic injury, and they are diagnosed with Barrett’s esophagus (BE). Some types of BE put patients at increased risk for developing esophageal cancer.
Most people with GERD can be successfully treated with a combination of lifestyle and dietary modifications, as well as medications. Lifestyle modifications include weight loss and stopping smoking. Other suggestions may include elevating the head of the bed on 6-inch blocks or sleeping on specially designed wedges that allow gravity to help minimize reflux of stomach contents into the esophagus during sleep. Recommended dietary changes are avoiding foods that can weaken the LES. This includes chocolate, caffeine, fatty foods, and alcoholic beverages. Avoiding foods with a high acid content (citrus fruits, tomatoes, and soft drinks) is also recommended.
Medications for GERD range from over-the-counter antacids that neutralize stomach acids, to more powerful medications that reduce the amount of stomach acid being produced. Some of these medications, often referred to as “H2 Blockers” or “Proton-pump Inhibitors”(PPIs), require a prescription.
Who Should Consider Surgery for GERD?
Surgery to relieve the symptoms of GERD is an option to consider if your gastroesophageal reflux symptoms are inadequately relieved with lifestyle/dietary modifications and an adequate trial of high-dose medical therapy. If you are unable or reluctant to continue lifelong medical therapy, you also may be a candidate for surgery. Women with significant osteoporosis particularly may be concerned with the long-term effects of PPI medications. Other patients who should consider surgery for GERD are those who have developed complications of GERD despite good medical therapy. These complications include strictures (narrowing) of the esophagus caused by chronic acid exposure and recurrent pneumonia caused by acid or food spilling into the lungs.
More information about GERD is available here.
The opinions expressed in this article are those of the author and do not necessarily reflect the views of The Society of Thoracic Surgeons.

