Adult Heart Transplantation
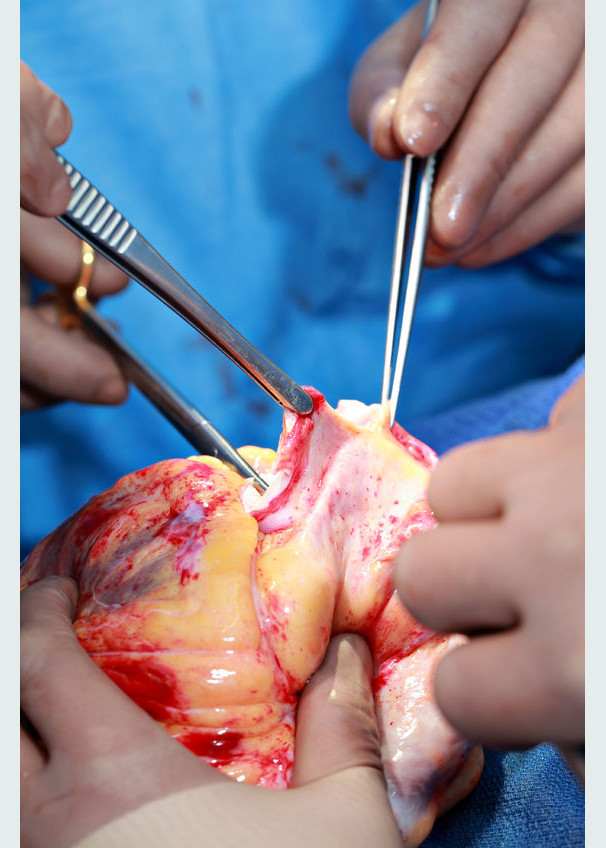
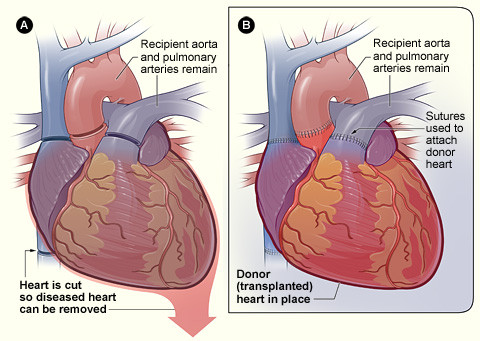
A heart transplant is an operation in which a medical transplant team, led by a cardiothoracic surgeon, will replace your failing heart with a new donor heart. Transplantation is usually considered a last option for patients with end-stage heart failure who cannot be treated with medication or other types of surgery.
The International Society for Heart and Lung Transplantation reports that more than 3,800 patients, including more than 500 children, receive new hearts each year. More than 3,500 lung transplants occur annually. Some patients require both a heart and lung transplant at the same time. Visit our page on lung transplantation for more information.
Survival rates for people receiving heart transplants continue to improve, especially in the first year after the transplant. About 88% of heart transplant patients survive the first year after surgery, and 75% survive for 5 years following transplant, according to the National Heart, Lung, and Blood Institute. The 10-year survival rate is about 56%.
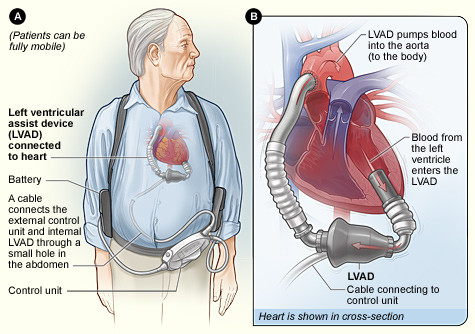
If you are ineligible for a heart transplant, your heart specialist also may consider using a ventricular assist device as a final treatment option. Ask your doctor for more information on VADs if you have been told you are unable to have a transplant.
The initial recovery period for heart transplantation is about 6 months. If you traveled out of state for your surgery, your transplant team may ask you to stay close to the hospital for a period of time after you are discharged so they can better monitor your recovery.