- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
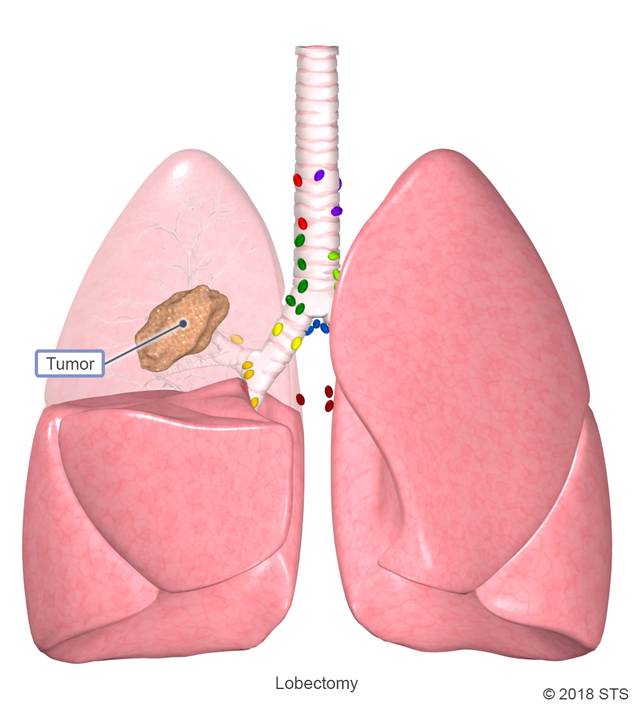
If you have certain chest and lung diseases, a lobectomy is a treatment option that your doctor may suggest. This operation is most commonly performed for early stage non-small cell lung cancer, when the tumor is located in just one part of the lung. Other conditions treated with a lobectomy include tuberculosis, emphysema, chronic obstructive pulmonary disease, lung abscesses, and benign tumors.
During a lobectomy, your cardiothoracic surgeon will remove the affected lobe so that disease doesn’t spread to the other lobes. Based on your diagnosis, the operation involves either a few small incisions (minimally invasive) or one longer incision (thoracotomy) on the side of your chest. After the surgery, your body adjusts to make up for the missing section. The remaining healthy lung tissue expands to fill the space and the other lung may shift toward the side of the removed lobe.
Before your operation, the doctor will want to make sure that you and your lungs are as healthy as possible. You will receive a physical exam and should be prepared to discuss your complete medical history, including your family history.
Preoperative tests
Preoperative tests, which may be conducted over several days and are necessary before your surgery, help your doctor be sure that your disease and health are suitable for the proposed operation. The tests may include:
Labs: Blood and urine tests help determine your overall health.
Imaging: A computed tomography (CT) scan helps provide more detail on your anatomy and disease.
Staging evaluation: If you have cancer, confirming the stage of disease is important to ensure that the right treatment is offered.
- Endobronchial Ultrasound (EBUS): During this outpatient, minimally invasive procedure, your doctor will examine and collect samples from your lungs and nearby lymph nodes in order to examine areas that need a closer look.
- Positron emission tomography (PET) scan: This imaging study helps determine if there are areas in the lung, lymph nodes, and elsewhere in the body that have increased activity related to tumor involvement.
- Brain magnetic resonance imaging (MRI): The MRI is a safe and painless test that uses a magnetic field and radio waves to produce detailed images of the brain, helping to establish if the tumor has spread to the brain.
Tests to assess your overall health and ability to undergo a lobectomy
- Cardiac evaluation: Your doctor may recommend an electrocardiogram (EKG), an echocardiogram (echo), or a referral to a cardiologist to ensure that you are safe to undergo surgery
- Lung function evaluation: This evaluation includes complete pulmonary function tests (see below for more information) to be sure that you will be able to have part of your lung removed without becoming short of breath or needing long-term oxygen.
For more information on these tests, visit our common diagnostic tests page.
Lung Function Tests
Breathing tests, known as pulmonary function tests, also will be performed to make sure you’ll be able to breathe adequately after a lobe of your lung is removed. These noninvasive tests include spirometry, a way of measuring your breaths.
In a spirometry test, while you are sitting, you breathe into the mouthpiece of a tube that is connected to machine called a spirometer. Keep in mind that a clip will be placed on your nose to keep your nostrils closed.

This test assesses how well your lungs work by measuring how much air you inhale, how much you exhale, and how quickly you exhale. A technician will give you specific instructions to breathe in deeply and breathe out as hard as you can. After the initial round of tests, you may receive inhaled medication to open your lungs and be asked to repeat the exercises. The breathing test, which takes about 5-10 minutes, may be performed at your doctor’s office or in a special cardiopulmonary center of a hospital.
Pulmonary rehabilitation
Based on the results of your pulmonary function tests, your doctor may suggest daily exercise or a pulmonary rehabilitation program to improve your breathing before the operation. Pulmonary rehabilitation is a personal program of education and exercise created by a team of doctors, nurses, physical therapists, respiratory therapists, exercise specialists, and dietitians. The goal? To increase awareness about your lungs and to help you achieve exercise and activity with less shortness of breath. Pulmonary rehabilitation also is possible after your operation.
Medications
Your doctor also will carefully review all of your medications. It is important to have ready a list of all of your current medications and any over-the-counter vitamins or herbal supplements that you are taking. Keep in mind that certain medications and supplements can increase the risk of bleeding, prolong the effects of anesthesia, or raise blood pressure during surgery, so your doctor may recommend stopping some well in advance of your operation.
Quit smoking
Very importantly, if you’re a smoker, your surgeon will strongly suggest that you quit as soon as possible—at least 3 weeks before surgery. Recent inhalation of even one cigarette paralyzes the cilia which are the little finger-like projections in your lungs that help clear your airways of secretions and prevent breathing complications after surgery. You’re considered a smoker if you have ever smoked or used any kind of tobacco product in the last 30 days. This includes e-cigarettes, vaporizers, and other types of electronic nicotine delivery systems. Be aware that inhalation of marijuana has the same detrimental effects on the lungs as inhalation of tobacco products. Quitting smoking before surgery can reduce your risk of complications, improve wound healing, and increase the chance that your surgery will be successful.

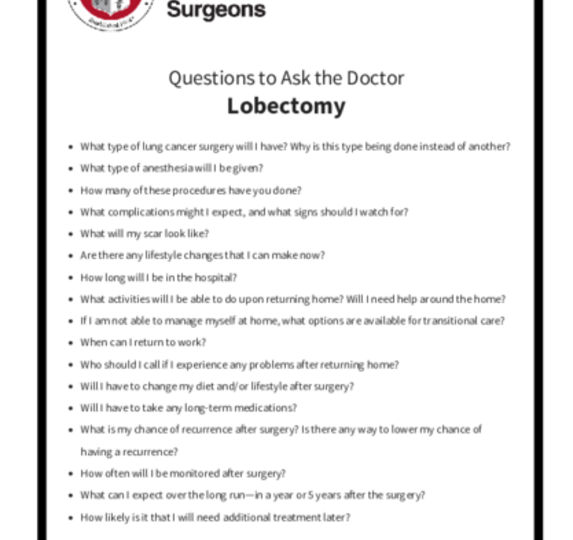
As you prepare for your lobectomy, you can take an active role by asking questions and educating yourself. In addition, taking steps to get organized at home and coordinate postoperative care can ease some of the anxiety you may feel in the weeks before surgery. Planning ahead may help improve your outcome as well.
You should:
- Arrange for transportation the day of your surgery. Several additional tests and administrative tasks must be done before you are ready for surgery, so it is very important to arrive on time.
- Find someone to help you at home with chores and errands during your first few weeks out of the hospital.
- Eat a healthy diet. Even if no specific recommendations are made, a diet rich in protein and certain nutrients can help you before surgery and aid in your recovery.
- Starting the night before surgery, you will be advised not to eat or drink anything until after your surgery. Follow your doctor’s instructions exactly, or your surgery may be canceled.
- Ask your doctor about any medications that you usually take in the morning, and if you should take them the morning of surgery.
- Choose comfortable clothes to wear while traveling to and from the hospital. Also, pack a bag with all of your basic essentials that you will bring to the hospital.
What can I expect on the day of surgery?
On the day of your lobectomy, your cardiothoracic surgeon will discuss with you what will happen in the operating room. This is a good time to ask any last minute questions that you may have. You also will meet with the anesthesiologist, who will review with you any previous complications or concerns that you have about undergoing general anesthesia. Your anesthesiologist will discuss the risks and benefits of anesthesia, as well as any possible side effects and complications. You’ll receive general anesthesia, which means you won’t be awake for the operation.
While waiting, you will probably have an intravenous (IV) line placed in your arm, and you may be given medication to relax you. The surgical staff will let your family know where they can wait so they can be updated on how your surgery is going and when it is finished.
Once you’re asleep, a tube is put into your windpipe through your mouth, a process called intubation. This tube is then attached to a ventilator that provides oxygen and helps you breathe. In addition, a soft, flexible tube called a catheter may be placed in your bladder to remove any urine. After you’re asleep, you also may have additional lines placed in your veins or in an artery of your arm to be used for monitoring. Your medical team will monitor your vital signs, such as blood pressure, heart rhythm, and blood oxygen levels during the operation.
Who is in the operating room?
Knowing who will be in the operating room with you can help put your mind at ease. In addition to your cardiothoracic surgeon, there likely will be several other people in the room, including:
- A surgical assistant who may be one of the surgeon’s partners, a physician assistant, or a cardiothoracic surgical resident who will help, as needed, during the operation
- An anesthesiologist who is in charge of administering anesthesia and monitoring vital signs
- A nurse anesthetist or anesthesia resident who may assist the anesthesiologist
- Nurses and technicians who assist the surgical team and prepare the operating room
What are the risks of lobectomy?
Lobectomy is a major surgery and may result in serious complications such as:
- Infections, for example pneumonia
- Prolonged air leak requiring the chest tube to be left in place longer than a few days. This is the most common complication.
- A collapsed lung, which prevents your lung from filling with air when you breathe in
- Bleeding
- An area of pus that forms in the chest cavity
- Fluid in the space between the lung and inner chest wall (pleural effusion)
- Heart problems such as a heart attack or irregular heart rhythms
- Blood clots in the legs that may travel to the lungs (pulmonary embolus)
- Post-thoracotomy pain syndrome
Your risks vary depending on your overall health and other factors. Be sure to discuss these possible risks with your surgeon before the operation.
Types of Lobectomy
Your cardiothoracic surgeon can perform the lobectomy in a few different ways. The surgical approach that is recommended for you depends on several factors, including:
- The location of the tumor
- The size of the tumor
- Whether or not the tumor has spread to nearby tissues
- Your overall health
- How well your lungs are functioning before surgery
In an open lobectomy, a lobe of the lung is removed through an incision on the side of the chest. This surgical approach is known as a thoracotomy.
The incision may be less than 3 inches to more than 8 inches long, depending on the type of access needed by the surgeon, the location and size of your tumor, and the type of access preferred by your surgeon. Most incisions are on the back under the shoulder blade, and may extend around your side and under your armpit. The incision will allow the cardiothoracic surgeon to gain access to the lung through the exposed ribs.
Before closing the incision, your surgeon will place at least one plastic drainage tube inside your chest cavity, with one end exiting your body through an incision on your side just under the breast. These tubes allow drainage of any extra fluids or air from the chest cavity. Chest tubes are usually removed within 2 days after surgery, but cannot be removed until the fluid volume is low enough and there’s no more air bubbling out of the tube.
A thoracotomy can take anywhere from 1.5 to 4 hours, depending on the complexity of your case. If your doctor uses an enhanced recovery pathway, the hospital stay may be 2 to 5 days.
In an open lobectomy, a lobe of the lung is removed through an incision on the side of the chest. This surgical approach is known as a thoracotomy.
The incision may be less than 3 inches to more than 8 inches long, depending on the type of access needed by the surgeon, the location and size of your tumor, and the type of access preferred by your surgeon. Most incisions are on the back under the shoulder blade, and may extend around your side and under your armpit. The incision will allow the cardiothoracic surgeon to gain access to the lung through the exposed ribs.
Before closing the incision, your surgeon will place at least one plastic drainage tube inside your chest cavity, with one end exiting your body through an incision on your side just under the breast. These tubes allow drainage of any extra fluids or air from the chest cavity. Chest tubes are usually removed within 2 days after surgery, but cannot be removed until the fluid volume is low enough and there’s no more air bubbling out of the tube.
A thoracotomy can take anywhere from 1.5 to 4 hours, depending on the complexity of your case. If your doctor uses an enhanced recovery pathway, the hospital stay may be 2 to 5 days.
In this minimally invasive procedure, a lobe of the lung is removed through small incisions in the chest. The ribs are not spread apart during a VATS. The cardiothoracic surgeon makes two to four incisions (up to 1.25 inches long) on the chest wall. A thin, rigid tube with a light and special camera (thoracoscope) and other small tools are placed through these cuts, allowing the surgeon to guide the tools while viewing the inside of the chest on a monitor.
Before closing the incision, your surgeon will place at least one plastic drainage tube inside your chest cavity, with one end exiting the body through an incision on your side just under the breast. The tubes allow drainage of any extra fluids or air from the chest cavity. Chest tubes are usually removed within 2 days after surgery, but cannot be removed until the fluid volume is low enough and there’s no more air bubbling out of the tube. The incisions are closed with sutures or staples. Because only small incisions are needed, you may have less pain, a shorter hospital stay (typically 2 to 5 days), and a faster recovery.
Even so, there are times when VATS is not possible. The location or size of some tumors makes it difficult to perform VATS, and in these cases, an open lobectomy might be safer and more likely to remove the whole tumor. Your surgeon may have various reasons for not offering you a VATS procedure. You can discuss with your surgeon whether or not you are a candidate for a VATS lobectomy.
In this minimally invasive procedure, a lobe of the lung is removed through small incisions in the chest. The ribs are not spread apart during a VATS. The cardiothoracic surgeon makes two to four incisions (up to 1.25 inches long) on the chest wall. A thin, rigid tube with a light and special camera (thoracoscope) and other small tools are placed through these cuts, allowing the surgeon to guide the tools while viewing the inside of the chest on a monitor.
Before closing the incision, your surgeon will place at least one plastic drainage tube inside your chest cavity, with one end exiting the body through an incision on your side just under the breast. The tubes allow drainage of any extra fluids or air from the chest cavity. Chest tubes are usually removed within 2 days after surgery, but cannot be removed until the fluid volume is low enough and there’s no more air bubbling out of the tube. The incisions are closed with sutures or staples. Because only small incisions are needed, you may have less pain, a shorter hospital stay (typically 2 to 5 days), and a faster recovery.
Even so, there are times when VATS is not possible. The location or size of some tumors makes it difficult to perform VATS, and in these cases, an open lobectomy might be safer and more likely to remove the whole tumor. Your surgeon may have various reasons for not offering you a VATS procedure. You can discuss with your surgeon whether or not you are a candidate for a VATS lobectomy.
Similar to VATS, robotic-assisted surgery is another minimally invasive procedure, but performed with robots. RATS allows the surgeon to operate through four to five small, half-inch incisions made between the ribs. No rib spreading is needed. A tiny 3D high-definition video camera is inserted into one of the incisions to give the surgeon a magnified, detailed view of the lung or inside of the chest. Surgical instruments are attached to robotic hands. The surgeon performs the operation while sitting at a console next to you. He/she uses hand and foot controls to guide the robotic hands, translating his/her movements into precise actions. This surgery can assist with hard-to-reach tumors. With RATS, you experience less pain and scaring, and recovery time is reduced. You can discuss with your surgeon whether or not you are a candidate for a RATS lobectomy.
For more information on robotic operations, read “Robotic Operations in Thoracic Surgery: Who Are the Candidates?”
Similar to VATS, robotic-assisted surgery is another minimally invasive procedure, but performed with robots. RATS allows the surgeon to operate through four to five small, half-inch incisions made between the ribs. No rib spreading is needed. A tiny 3D high-definition video camera is inserted into one of the incisions to give the surgeon a magnified, detailed view of the lung or inside of the chest. Surgical instruments are attached to robotic hands. The surgeon performs the operation while sitting at a console next to you. He/she uses hand and foot controls to guide the robotic hands, translating his/her movements into precise actions. This surgery can assist with hard-to-reach tumors. With RATS, you experience less pain and scaring, and recovery time is reduced. You can discuss with your surgeon whether or not you are a candidate for a RATS lobectomy.
For more information on robotic operations, read “Robotic Operations in Thoracic Surgery: Who Are the Candidates?”
What happens after a lobectomy?
When you wake up from surgery, you will feel groggy. You will be taken to a recovery room, and then to a surgical unit. Depending on the hospital, you may be on a special unit just for patients who have had lung surgery. Your heart rate, blood pressure, and oxygen levels will be checked regularly during this time.
Through your IV, you’ll receive fluids and medications. You may have a catheter in your bladder to drain urine, which will be removed when you’re able to get up and use the bathroom on your own. The chest tube, which may cause pain when you move, cough, or breathe deeply, will remain in place for approximately 2 days after the operation. A chest x-ray will be done right after the surgery, and may be repeated multiple times throughout your hospital stay. This is to make sure your lungs are okay.
A respiratory therapist will teach you coughing methods to help your lungs re-expand after surgery and to prevent pneumonia. You also will do deep-breathing exercises using the hand-held incentive spirometer. It’s possible that you may need oxygen for some time after surgery. In most cases, the oxygen will be stopped before you go home.

You will be expected to get up and walk around, and will be encouraged to stay out of bed as much as possible starting the day after your operation. This will help your lungs heal faster and prevent blood clots in your legs. You will have some pain, which can be controlled with medications and usually subsides within 2 to 4 weeks. The nurse will ask you about your pain often and give you medication as needed. It’s important to control your pain so you can cough, breathe deeply, use your incentive spirometer, and get out of bed and walk.
You can expect to stay 3 to 5 days in the hospital, depending on the type of lobectomy that was performed and whether or not your hospital/surgeon uses an enhanced recovery protocol. Upon discharge, you will be given specific incision care instructions and plans for a follow-up appointment with your surgeon. Most patients are back to their normal routines within 1 month after surgery.
Recovery at home
Healing after a lobectomy takes time. For the first several weeks, you’ll probably feel tired often. This is because your body is using a lot of energy to heal itself. Be patient; your fatigue will improve with time. You may find that it is difficult to allow people to help, but delegating some tasks and learning to accept assistance may help you recover faster.
It is not uncommon to experience anxiety or depression after lung surgery. If you are feeling especially worried or stressed, reach out to your treatment team, family, and friends. You also may want to consider joining a support group or talking with a professional counselor.
For a more information on what to expect after surgery, read “What Patients Should Know About Life After Lung Cancer Surgery.”
Medications
Your doctor will prescribe medications to manage pain during recovery. You should take the medication exactly as directed and as needed. This is an important part of your care after surgery. As your incisions heal, you will have less pain and need less pain medication.
Another option to minimize pain after surgery is an enhanced recovery program. This patient-centered program is designed to help you recover more quickly and lower the chances that you will experience problems after your operation. Talk to your surgeon and health care team about whether an enhanced recovery program is available and if it would benefit you during your recovery.
Side effects
You will receive instructions on how to deal with common side effects from surgery such as:
- Discomfort or itching from healing incisions
- Muscle pain or tightness in the shoulders and chest
- Fatigue (tiredness), mood swings, or depression
- Problems sleeping or loss of appetite
- Constipation
Side effects often go away within 4 to 6 weeks.
Most wound infections develop within 14 days of the surgery. If you develop any of the following signs or symptoms, you should contact your doctor immediately:
- Fever greater than 100.4° F
- New or worsened pain in the chest or around the incision
- A rapid heart rate
- Feeling short of breath
- Pain with or trouble breathing
- Chest pain
- Reddened skin, bleeding or pus-like drainage from the incision
- Confusion or other change in mental state
- Green, yellow, or blood-tinted phlegm
Physical activity
Keep doing the breathing and coughing exercises that you learned in the hospital. In addition, slowly increase your physical activity as you can handle it. It’s important that you don’t simply sit in bed or on the couch all day once you leave the hospital. Even if you’re only able to walk for a few minutes at a time, getting up and doing so regularly can help your recovery.
As you grow stronger, try to walk for longer periods of time, but be careful not to wear yourself out. Normal, everyday activities may be tiring for you, so listen to your body; it is an excellent guide for telling you when you have done too much. A good goal is to move for at least 30 minutes a day. This will help you regain your strength and keep your lungs healthy and clear.
Also important while you’re healing is to prevent exposure to:
- People with colds, sore throats, or the flu
- Tobacco smoke
- Chemical fumes
- Environmental pollution
Ongoing Care
Care after your lobectomy will include periodic checkups with your doctors. Your first appointment after surgery likely will be within 4 weeks of your operation. During the visit, various tests, such as a chest x-ray, may be done to see how your lungs are working.
Read more about recovery after lung cancer surgery in the blog article, “You’ve Had Lung Cancer Surgery: Now What?”
Also available is a blog article that discusses common myths about lung cancer surgery.
Reviewed by: Mara B. Antonoff, MD
July 2019