- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
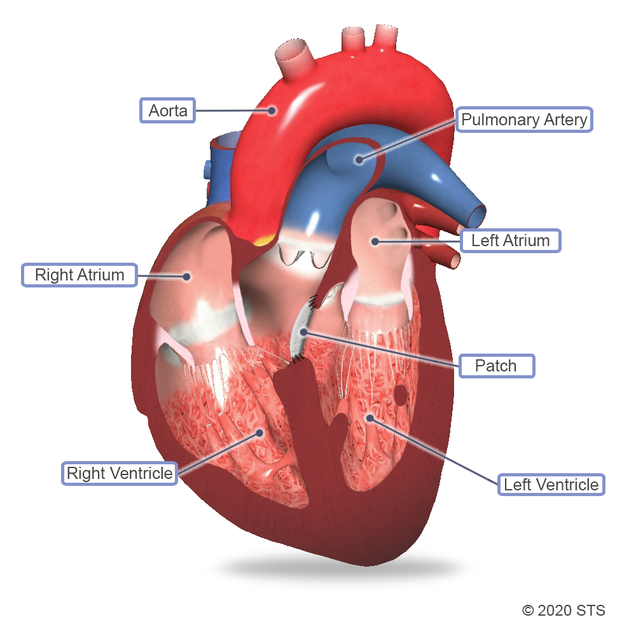
A ventricular septal defect (VSD) is a common heart defect that affects an estimated 42 out of every 10,000 babies born annually, according to the US Centers for Disease Control and Prevention. With a VSD, there is an abnormal opening in the wall between the main pumping chambers of the heart (the ventricles).
VSD repair is a type of heart operation that is performed to close a VSD, which is sometimes referred to as a “hole in the heart.” According to The Society of Thoracic Surgeons National Database (which includes more than 95% of all congenital heart surgery hospitals in the US and Canada), approximately 7,500 VSD surgeries were performed in 2018 (the most recent year available). Not all VSDs will require surgical closure, and your cardiologist will advise you on how to proceed.
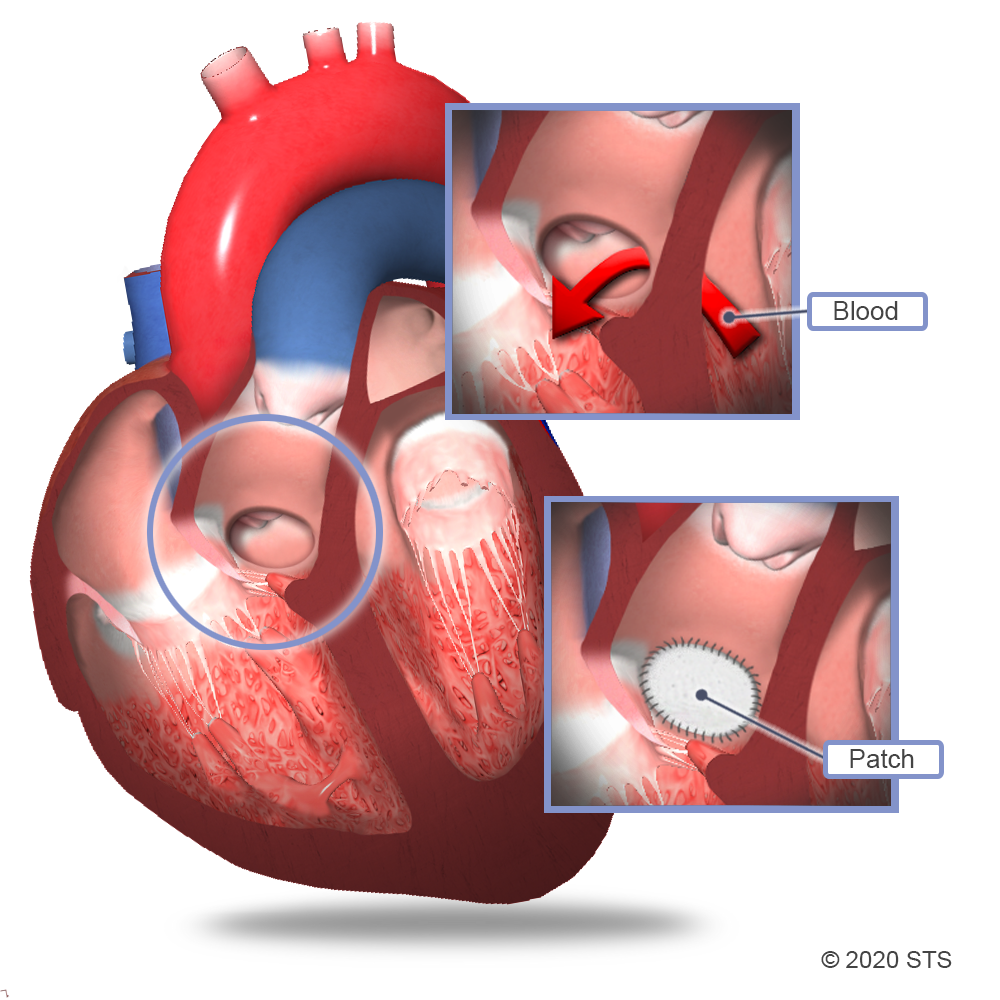
In normal development, the walls (septum) between the heart chambers connect, separating the four chambers before the baby is born. But sometimes, this doesn’t happen. When there is a hole, blood is allowed to pass from the left side of the heart to the right side, causing too much oxygen-rich (red) blood to get pumped back to the lungs instead of out to the body. The result? The extra blood pumped into the lung arteries makes the heart and lungs work harder. The lungs can become congested and be permanently damaged.
In most cases, the operation is performed within the first few years of a child's life. If the hole is large enough to cause a newborn to have symptoms (described below), a surgery may be needed in the first weeks to months of life.
Treatment of a VSD depends on a child’s age, as well as the size, location, and severity of the hole.
It’s important to note that VSDs do not get bigger, but sometimes they will get smaller or close completely on their own without any treatment. For this reason, the doctor may not immediately recommend surgery, but will watch your child closely and treat any symptoms with medication.
In general, small VSDs usually don’t cause symptoms and are more likely to close on their own. Many small VSDs will do so before your child is 2 years old.
Medium and large VSDs often result in noticeable symptoms such as fast breathing, tiring easily, poor feeding, and failure to gain weight and grow properly. These signs typically indicate that the VSD will not close by itself. In this case, your doctor may recommend heart surgery to fix the hole. The purpose of this surgery is to ease symptoms caused by the VSD and prevent long-term damage to the heart and lungs.
While infants and children most often receive this type of operation, adults sometimes also need the surgery if their VSD was not diagnosed during childhood.
Be sure to speak with your doctor about what treatment is right for your child. If surgery is recommended, your doctor will refer you to a cardiothoracic surgeon.
Once your child has been referred for heart surgery, you will have the opportunity to meet with the care team and the cardiothoracic surgeon. They will explain the operation and what will be done to help your child.
If you have questions about your child’s condition or the operation, make sure to ask those questions until you feel comfortable that you understand the answers. In addition, it is essential that you share with the surgeon a list of all medications that your child is taking, especially if he/she is on blood thinners (anticoagulants). These can lead to excess bleeding during and after surgery, and usually need to be stopped before the scheduled operation.
Medication may be prescribed to reduce your child’s symptoms before surgery. In addition, the doctor may request preoperative tests to help assess your child’s overall health and ability to undergo a VSD operation. The tests may include:
- Chest x-ray: provides a black-and-white image of the lungs and heart
- Electrocardiogram (EKG): shows the pattern and rate of your child’s heart rhythm
- Blood tests: check general health
- Echocardiogram (echo): uses sound waves (ultrasound) to create detailed pictures of the heart anatomy and its blood flow
For more information on these tests, visit the common diagnostic tests page .
Some hospitals offer tours of the Intensive Care Unit (ICU) and post-operative hospital wards, where your child will recover after surgery. You are encouraged to familiarize yourself with the hospital, its surroundings, and its resources in order to become comfortable with the environment.
For more information on what to expect before your child’s surgery, visit “Before Congenital Heart Surgery.”
What can I expect on the day of surgery?
On the day of the surgery, be sure to arrive at the hospital promptly at your assigned time. Once your child is checked in, a nurse from the care team will be available to help guide you through the steps. You can expect to see the cardiothoracic surgeon who will discuss with you what will happen in the operating room (OR). This is a good time to ask any last-minute questions that you may have.
Your child will receive general anesthesia, which means he/she won’t be awake for the operation; so you also will meet with the anesthesiologist, who will review any concerns that you have about your child undergoing anesthesia. The anesthesiologist will discuss the risks and benefits of anesthesia, as well as any possible side effects and complications.
A nurse will bring your child to the OR, often along with the anesthesiologist. After your son/daughter has been taken into surgery, you will be asked to sit in the designated parent waiting area. The surgeon will meet with you there after the operation. Some hospitals are able to offer communication through text on your mobile phone to allow you more freedom to leave the waiting area during the surgery.
Who is in the operating room?
Knowing who will be in the operating room with your child can help put your mind at ease. In addition to the cardiothoracic surgeon, there likely will be several other people in the OR, including:
- A surgical assistant who may be one of the surgeon’s partners, a physician assistant, or a cardiothoracic surgical resident who will help, as needed, during the operation
- An anesthesiologist who is in charge of administering anesthesia and monitoring vital signs
- A nurse anesthetist or anesthesia resident who may assist the anesthesiologist
- Nurses and technicians who assist the surgical team and prepare the operating room
What are the risks of VSD surgery?
Most children who have VSD surgery do not experience any complications. However, all operations have risks. For VSD surgery, the risks include:
- Excess bleeding
- Infection
- Blood clot, which can increase the chances of stroke or other problems
- Abnormal heart rhythm
- Heart block, which can make a pacemaker necessary
- Valve injury (tricuspid, pulmonary, or aortic)
- Complications from anesthesia
Ask the doctor about possible risk factors for your child.
What happens during VSD surgery?
For the surgery, your child will receive general anesthesia so he/she will be in a deep sleep during the operation and not feel any pain. The cardiothoracic surgeon will make an incision down the middle of the chest and separate the breastbone to reach the heart. Your child will be connected to a heart-lung machine that pumps blood and acts as the heart and lungs during the surgery.
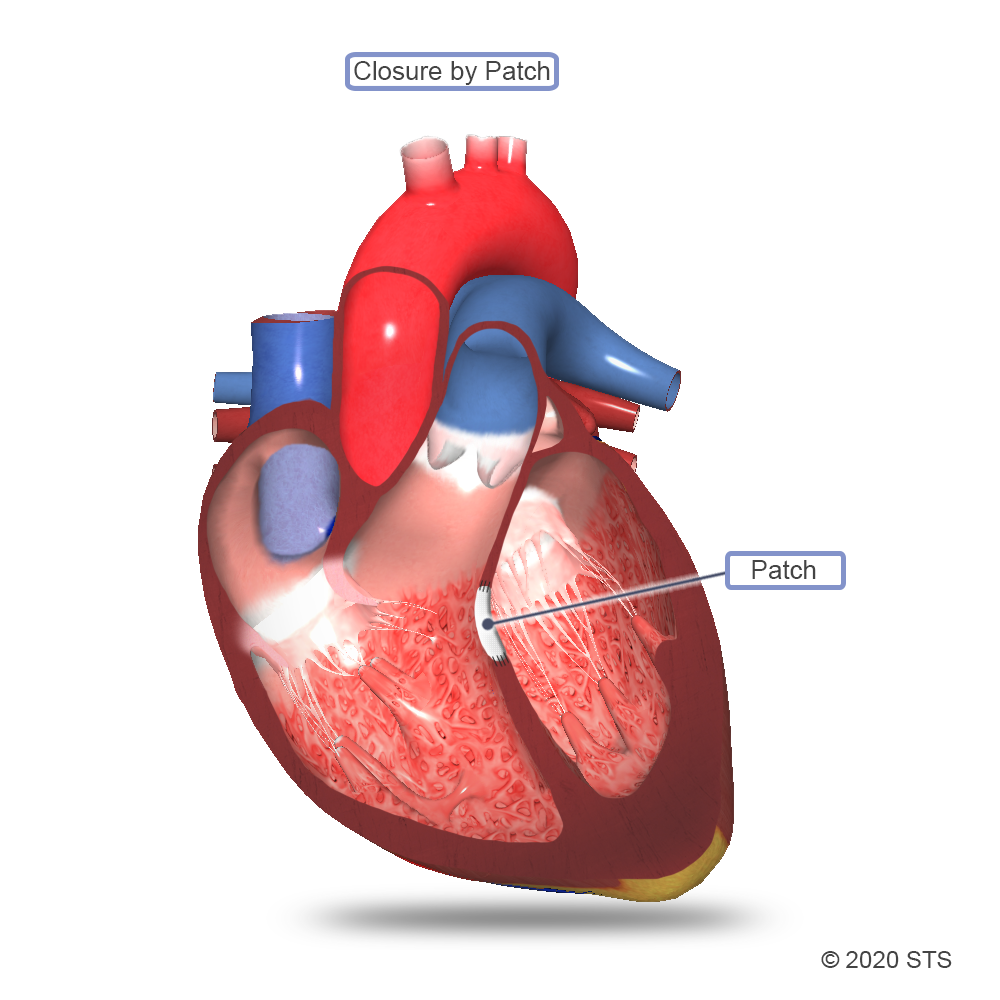
Most commonly, a tightly woven patch of manmade surgical material is sewn over the hole. Heart tissue will grow over the patch and, usually by 6 months after the surgery, the hole will be covered completely with normal heart lining tissue. Sometimes, the surgeon will stitch the hole closed directly, without the use of a patch, or use your child’s own tissue called pericardium (the sac that surrounds the heart).
Once the surgery is completed, the heart-lung machine will be removed. The surgeon will put your child’s breastbone and skin back together. A bandage will be placed over the incision once it’s closed. You can expect the surgery to take several hours.
Most commonly, a tightly woven patch of manmade surgical material is sewn over the hole. Heart tissue will grow over the patch and, usually by 6 months after the surgery, the hole will be covered completely with normal heart lining tissue. Sometimes, the surgeon will stitch the hole closed directly, without the use of a patch, or use your child’s own tissue called pericardium (the sac that surrounds the heart).
Once the surgery is completed, the heart-lung machine will be removed. The surgeon will put your child’s breastbone and skin back together. A bandage will be placed over the incision once it’s closed. You can expect the surgery to take several hours.
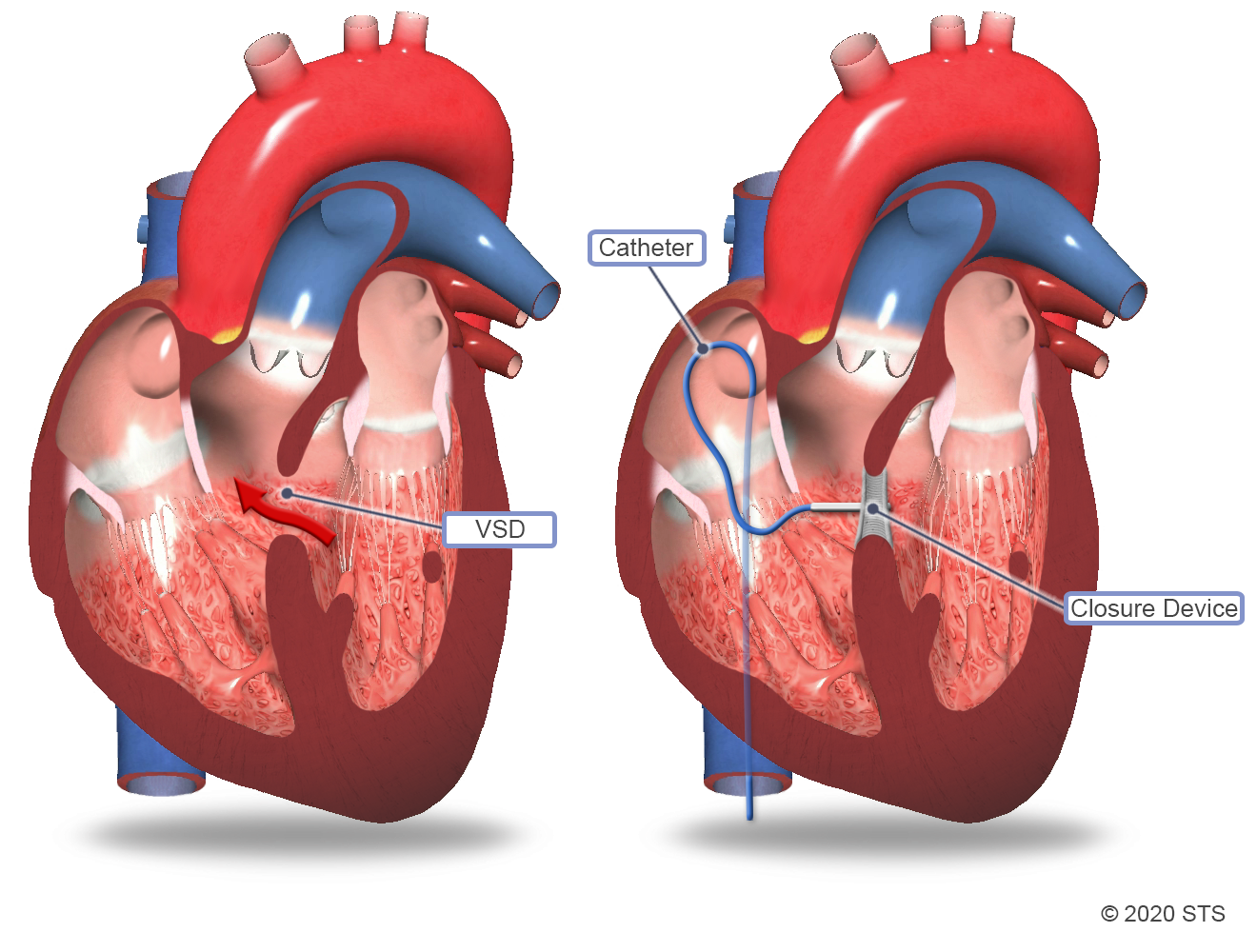
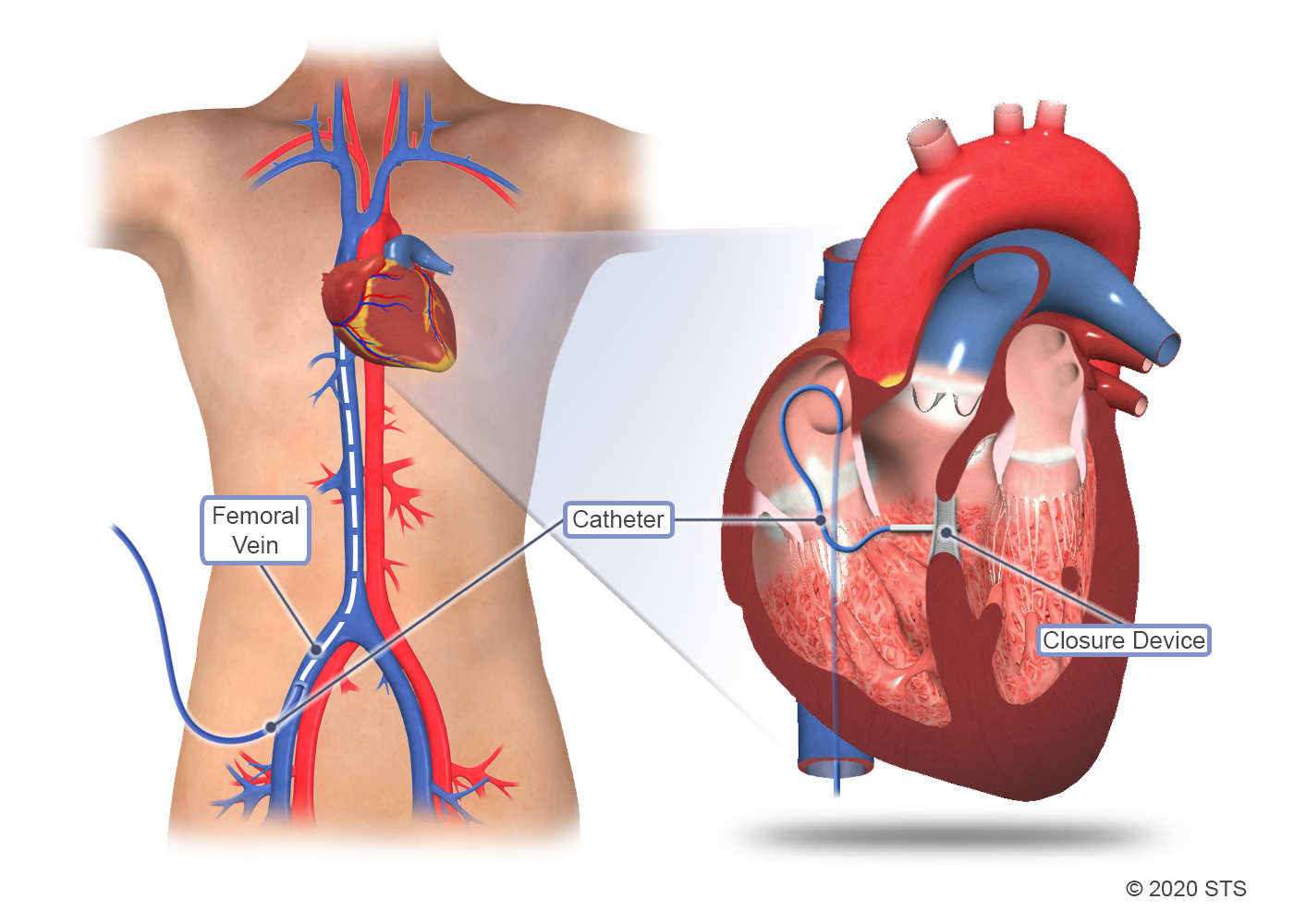
Although surgery is the standard of care for VSD, your doctor may recommend a minimally invasive catheter-based procedure instead. During this type of procedure, an interventional cardiologist will insert a thin, flexible tube (catheter) in a blood vessel in the upper thigh and guide the catheter to your child's heart. A specially sized wire mesh implant will be passed through the catheter and plugged into the hole to permanently block blood flow through the VSD.
Although surgery is the standard of care for VSD, your doctor may recommend a minimally invasive catheter-based procedure instead. During this type of procedure, an interventional cardiologist will insert a thin, flexible tube (catheter) in a blood vessel in the upper thigh and guide the catheter to your child's heart. A specially sized wire mesh implant will be passed through the catheter and plugged into the hole to permanently block blood flow through the VSD.
Sometimes, the VSD surgery is performed using a combination of the surgical and catheter-based techniques (hybrid procedure). For a hybrid procedure, the surgeon will place a wire mesh device over the VSD using a catheter that is threaded through a small incision. This procedure may be performed without using the heart-lung machine.
Sometimes, the VSD surgery is performed using a combination of the surgical and catheter-based techniques (hybrid procedure). For a hybrid procedure, the surgeon will place a wire mesh device over the VSD using a catheter that is threaded through a small incision. This procedure may be performed without using the heart-lung machine.
What happens after VSD surgery?
In most cases, your child will go to the ICU immediately after the operation. There, a specialized team of experts in pediatric heart care will watch over your child, assisted by the most sophisticated monitoring equipment available.
Your child may remain sedated and on a breathing machine after the operation until it is safe to breathe on his/her own. You may notice small catheters inserted into arteries and veins. These help measure blood pressure and administer medications. Pain medicine and sedatives will be given in order to keep your child as comfortable as possible. Your child also may have small chest tubes that drain a normal amount of bloody fluid and help keep the lungs expanded. The ICU staff will keep you informed about your child’s progress and explain the plan of care and equipment. Feel free to ask questions.
Read the article, “Preparing for Your Child’s Heart Surgery: Life in the Cardiac ICU,” to learn more about what to expect when your child is in the ICU.
When the care team thinks your child no longer needs intensive monitoring, he/she will be transferred to the step-down unit. The staff in this unit has special training in the care of children who have had heart surgery. The cardiothoracic surgeon, cardiologist, nurse practitioner, nurse care manager, and care coordinator will continue to monitor and plan your child’s care until discharge. Your child should be able to go home approximately a week after surgery.
What else do I need to know?
- The doctor may prescribe medication to manage pain during recovery. Make sure your child takes the medicine exactly as directed and as needed. This is an important part of his/her care after surgery.
- Follow all of the instructions from your child’s care team about medicine, diet, and incision care.
- Your son/daughter will return to the hospital for at least one checkup with the surgical team within 1-2 weeks of going home. During this appointment, the surgeon will check your child’s incision and remove any remaining stitches.
- You also will need to schedule a follow-up appointment with the cardiologist in the first few weeks after the surgery. The doctor will monitor the VSD repair and look for signs or symptoms of any problems. It’s possible that your child may have another echocardiogram to make sure that the VSD has closed completely.
- Ask about your child’s risk of endocarditis (infection of the heart valves). The doctor may recommend that your child receives antibiotics before certain dental procedures for a period of time after VSD repair.
Recovery at home
In most cases, children who have had VSD surgery recover quickly and without complications. Most children can get back to their normal activities when they return home. The doctor can advise you about which activities are safe for your child. Keep in mind that many children with VSDs lead healthy, fully active, productive lives. But keep in mind that your child may tire more easily for a while. His/her body is using a lot of energy to heal itself.
If your child develops any of the following signs or symptoms, you should contact your doctor or go to the emergency room immediately:
- Trouble breathing
- Bluish color around the mouth or on the lips and tongue
- Poor appetite or difficulty feeding
- Failure to gain weight or weight loss
- Listlessness or decreased activity level
- Long-lasting or unexplained fever greater than 100.4° F
- Increased pain, tenderness, or pus-like drainage from the incision (a little drainage from the site is normal)
It is not uncommon to feel especially worried or stressed about your child’s surgery and recovery. You may want to consider reaching out to your treatment team, family, and friends, joining a support group for families of children born with heart defects, or talking with a professional counselor.
Visit “After Congenital Heart Surgery” for more information on your child’s recovery after VSD surgery.
For more information about congenital heart defects, read “Five Questions Parents Ask About Heart Defects.”
Reviewed by: Lauren G. Kane, MD
March 2020