- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
Failure does not mean that the heart has stopped working completely, but that the heart muscle has weakened over time and cannot pump blood as strongly as it once could.
According to the National Heart, Lung, and Blood Institute (NHLBI), heart failure is very common, affecting about 5.7 million people in the United States.
Heart failure usually develops slowly over time, as certain conditions, such as narrowed arteries in your heart (coronary artery disease), high blood pressure (hypertension), diabetes, viral infections, heart valve disease, and alcohol or drug use, gradually weaken your heart so that it works less efficiently.
One way to reduce your risk of heart failure is to control these health conditions.
Lifestyle changes, such as exercising, reducing salt in your diet, managing stress, losing weight, and not smoking, also can reduce your risk of developing heart disease and improve your quality of life.
Heart failure also can develop following a heart attack or when one of your heart valves becomes defective or diseased as you age.
Heart failure can start very suddenly (acute), such as from a heart attack, or it may develop slowly over time (chronic).
Common symptoms of heart failure include shortness of breath (dyspnea), especially when lying down, fatigue and weakness, swelling in your legs and ankles, or a rapid or irregular heartbeat.
Other symptoms include:
- Persistent cough
- Loss of appetite
- Nausea
- Confusion or impaired thinking
- Difficulty maintaining level of exercise
- Swelling/fluid buildup in the abdomen (ascites)
- Racing heart (palpitations)
You also may experience chest pain if your heart failure is caused by narrowed coronary arteries.
As a first step, your doctor will perform a physical exam and evaluate your overall health and any symptoms you are experiencing. In addition to the physical exam, your doctor will order a series of tests to confirm a heart failure diagnosis. Often, blood tests are used to check your kidney, liver, and thyroid function and to look for indicators of other diseases that affect the heart.
Your doctor also may recommend one or more of the following tests: electrocardiogram (EKG), chest x-ray, echocardiogram (echo), stress test, blood tests, or coronary angiography. For more information on these tests, visit our common diagnostic tests page.
Currently, heart failure has no cure. However, certain medications, treatments, and lifestyle changes can help you live a longer, more active life.
If your heart failure cannot be managed through medication, and diet and lifestyle changes, you likely will require surgery to treat certain problems. Heart failure may be improved by coronary artery bypass surgery, which improves blood flow to the heart muscle or by repairing or replacing damaged heart valves. In very severe cases, mechanical heart pumps can be used to assist heart function. If your heart cannot be repaired, it may have to be replaced through heart transplantation.
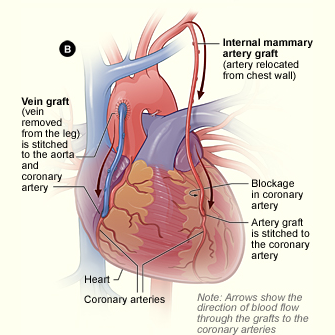
A common surgery used to treat heart failure is coronary artery bypass grafting surgery (CABG; often pronounced “cabbage”). It is the most commonly performed “open heart” operation in the United States.
A cardiothoracic surgeon will make an incision down the front of your chest, through your breastbone or sternum, and will then take a healthy blood vessel, usually from your leg, arm, or chest, and connect it to the other arteries in your heart. This enables blood flow to “bypass,” or go around, the diseased or blocked portion of your coronary artery, creating a new path for blood flow to your heart muscle.
A common surgery used to treat heart failure is coronary artery bypass grafting surgery (CABG; often pronounced “cabbage”). It is the most commonly performed “open heart” operation in the United States.
A cardiothoracic surgeon will make an incision down the front of your chest, through your breastbone or sternum, and will then take a healthy blood vessel, usually from your leg, arm, or chest, and connect it to the other arteries in your heart. This enables blood flow to “bypass,” or go around, the diseased or blocked portion of your coronary artery, creating a new path for blood flow to your heart muscle.
During valve surgery, the cardiothoracic surgeon makes a 6- to 8-inch long incision down the center of your sternum (breastbone) to open the chest, providing direct access to your heart. The damaged valve or valves may be repaired or replaced depending on the severity of valve damage. Correcting valve disease allows more normal blood flow through the heart chambers.
During valve surgery, the cardiothoracic surgeon makes a 6- to 8-inch long incision down the center of your sternum (breastbone) to open the chest, providing direct access to your heart. The damaged valve or valves may be repaired or replaced depending on the severity of valve damage. Correcting valve disease allows more normal blood flow through the heart chambers.
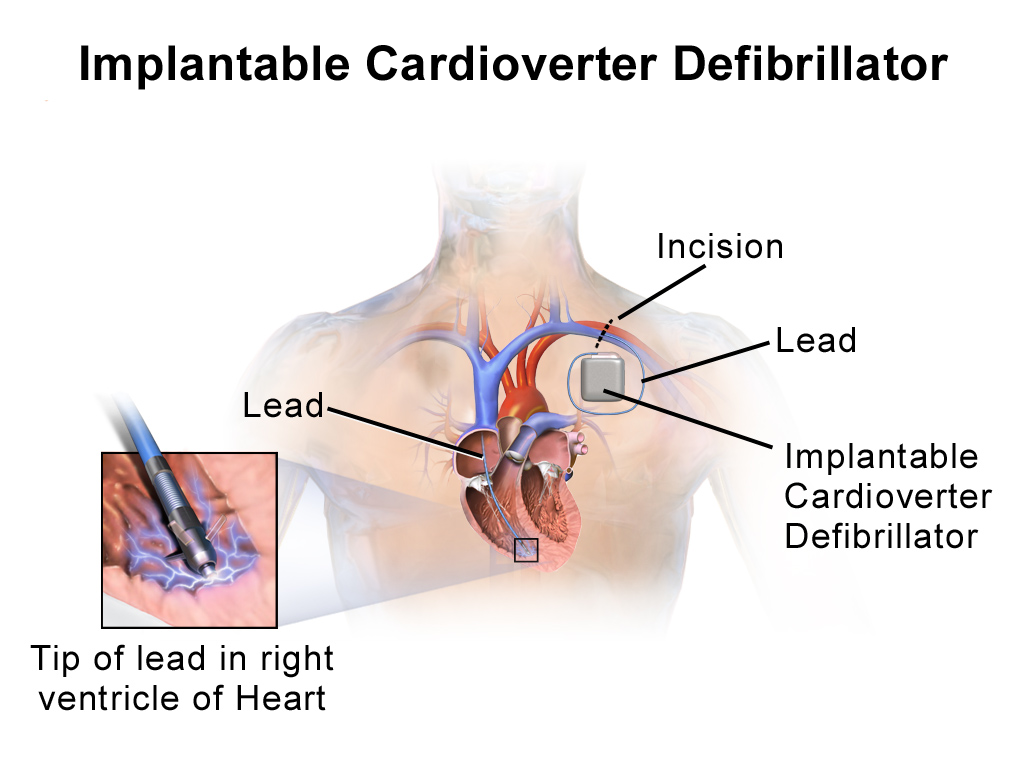
A surgeon also may be able to implant a medical device to help control your heart failure, such as an implantable cardioverter-defibrillator (ICD).
An ICD is similar to a pacemaker and is implanted under the skin in your chest. The device has wires that connect into your heart through your veins, which enables it to monitor your heart rhythm. An ICD also can function as a pacemaker and speed up your heart if necessary.
A surgeon also may be able to implant a medical device to help control your heart failure, such as an implantable cardioverter-defibrillator (ICD).
An ICD is similar to a pacemaker and is implanted under the skin in your chest. The device has wires that connect into your heart through your veins, which enables it to monitor your heart rhythm. An ICD also can function as a pacemaker and speed up your heart if necessary.
If you have a device implanted, you will require follow-up and monitoring by a heart specialist. Be sure to speak with your doctor prior to surgery to develop an initial recovery plan so that you know what to expect in the first few days and weeks following surgery.
Your doctor also may recommend that you:
- Reduce alcohol consumption
- Quit smoking
- Stay active and increase your activity level (be sure to speak with your doctor before starting any exercise or fitness program)
- Lose weight if you are overweight
- Lower bad cholesterol
- Get more rest
- Closely monitor other medical problems, such as lung or thyroid disease
It is important that you follow your treatment plan and take all medications as prescribed by your doctor. Make sure you understand your doctor’s advice and talk with your pharmacist about all of the medications you are taking. You can print these sample questions to use as a basis for discussion with your doctor.
Getting medical care for other health conditions, like diabetes or high blood pressure also is important. Ask your doctor about how often you should have your blood sugar level and blood pressure checked, and if you can measure these levels at home on your own.
Following a heart healthy diet also will help manage your heart failure. Ask your doctor to help you develop a plan or to recommend a nutritionist who can help put together a low sodium, low fat diet.
Reviewed by: Robbin G. Cohen, MD
June 2016
Previously reviewed by: Emily A. Farkas, MD