- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
Your care team will give you specific instructions on how to prepare the day of your surgery.
Check with your doctor to see if you can drink water in order to take any necessary medications. You also should ask about any medications you usually take in the morning, and if you should take them the morning of surgery. Make sure to brush your teeth, as bacteria in your mouth can increase your risk of pneumonia.
The night before your surgery and again in the morning, use an unscented, antibacterial soap when showering or bathing. Your doctor may provide more detailed instructions on how to prepare the surgical area.
You’ll generally need to arrive at the hospital at least 2 hours before your surgery. Your surgeon’s office or the hospital operating room will tell you when to arrive. You may want to map out your route prior to that day so you can anticipate traffic problems. Make sure you bring identification, insurance information, and items to make you comfortable during your stay, such as slippers, loose-fitting clothing, and personal care items. Don’t bring anything valuable.
Other important things to remember:
- Don’t wear any lotion, cream, deodorant, makeup, powder, perfume, or cologne.
- Remove all jewelry.
- If you wear contact lenses, wear your glasses instead.
Your family members generally will be allowed to stay with you while you meet with your medical team and wait for your operation. Once you’re ready for surgery, they will be directed to a waiting area where they will receive updates throughout your surgery and will be called when your operation is over. When it’s time to change for surgery, you will receive a hospital gown, robe, and nonskid socks to wear.
You will be completely asleep (general anesthesia) during your operation. You will meet with the anesthesiologist, who will review with you any previous complications or concerns that you have about undergoing general anesthesia. Your anesthesiologist will discuss the risks and benefits of anesthesia, as well as any possible side effects and complications. Possible side effects may be nausea and vomiting, but medication to treat these symptoms can be given, if needed. Your anesthesiologist or nurse will place an intravenous (IV) line in order to give you fluids and pre-medications.
When your surgical team is ready, you will be taken to the operating room where your anesthesiologist will begin administering general anesthesia through the IV. Under general anesthesia, you are in a state of controlled unconsciousness during which you are asleep and feel nothing. Once you’re asleep, a tube is put into your windpipe through your mouth, a process called intubation. This tube is then attached to the ventilator or breathing machine to provide oxygen and breaths during the operation and potentially during the early stages of recovery. It is usually removed as you wake up from surgery. In addition, a soft, flexible tube called a catheter will be placed in your bladder to remove any urine. The catheter will still be in place when you wake up after surgery.

Knowing who will be in the operating room (OR) with you before arriving at the hospital can help put your mind at ease. In addition to your cardiothoracic surgeon, there likely will be several other people in the OR, including:
- Surgical Assistant – One of your surgeon’s partners, a physician assistant, or a cardiothoracic surgical resident (if your surgery is at a university medical center) will help, as needed, during the operation.
- Nurses – Two or three nurses will handle the surgical instruments and provide supplies.
- Anesthesiologist – The anesthesiologist will monitor your sedation and pain medication levels throughout the surgery.
Before the operation, your surgeon will have discussed with you how your operation will be performed and which type of incision you will have. He/she can take a few different approaches to removing the lung cancer, depending on the specifics of your disease and your overall health. You can expect the surgery to take up to 6 hours.
Wedge Resection/Segmentectomy
These procedures remove only the cancerous part of the lobe, rather than the entire lobe.
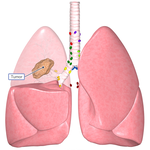
Lobectomy
This procedure removes an entire lobe of the lung and is the standard treatment for early stage lung cancers.
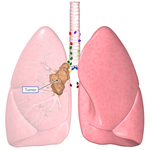
Pneumonectomy
This procedure removes an entire lung.
All of these operations can be performed in different ways, including:
- Open surgery (thoracotomy): A large incision is made around one side of the back, underneath the shoulder blade. This type of surgery is typically used when removing the entire lung.
- Video-assisted thoracic surgery (VATS): With this surgery, one or more small incisions are made on your side, back, or both so that a long, thin video camera and surgical tools can be inserted. This type of surgery is used to remove lobes or sections of the lungs. VATS may reduce the amount of time you need to spend in the hospital after surgery and may help you return to your normal activities sooner.
- Robotic-assisted thoracic surgery: This minimally invasive procedure is used to remove cancerous cells and may be helpful assisting with hard-to-reach tumors. A tiny video camera is inserted through a few tiny incisions between the ribs. Surgical instruments attached to a robotic hand are used during the procedure, with your surgeon guiding the hand while seated at a control unit. Learn more from Dr. Linda Martin in her blog post, “Robotic Operations in Thoracic Surgery: Who Are the Candidates?”
During the operation, you will have a chest tube inserted to help drain excess air and fluid and to help your lungs re-inflate. It’s likely that this tube will remain in place for a few days. The tube will be connected to a device that measures the amount of fluid coming out and checks if your lung is leaking air. The tube will be removed when the fluid output is low and your lung is not leaking air. Your incisions will be closed with sutures (stitches), in addition to thin pieces of surgical tape or surgical glue. The incisions also may be covered with bandages.
Learn more about what to expect After Lung Cancer Surgery.
Read more about Lung Cancer.
Reviewed by: Robbin G. Cohen, MD
October 2018