- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
End-stage lung disease can be caused by a variety of diseases including:
- Chronic obstructive pulmonary disease (COPD) or emphysema
- Scarring of the lungs (pulmonary fibrosis)
- Cystic fibrosis (CF)
- Pulmonary vascular disease (primary pulmonary hypertension)
These diseases and conditions can affect the flow of air and blood into and out of your lungs as well as gas exchange in the air sacs, or alveoli, of the lung.
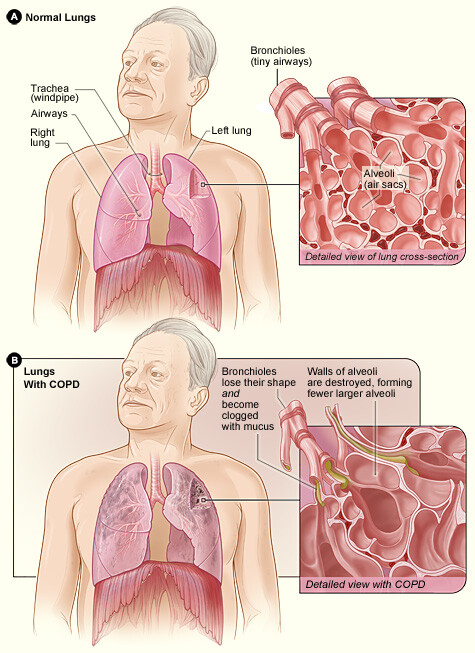
Chronic obstructive pulmonary disease
COPD, which includes chronic bronchitis and emphysema, is a lung disease that makes it hard to breathe. It often develops slowly and gets worse over time. The leading cause of COPD is cigarette smoking but long-term exposure to other lung irritants, such as air pollution, chemical fumes, or dust, also may contribute to COPD. COPD can cause coughing that produces large amounts of mucus, wheezing, shortness of breath, and chest tightness.
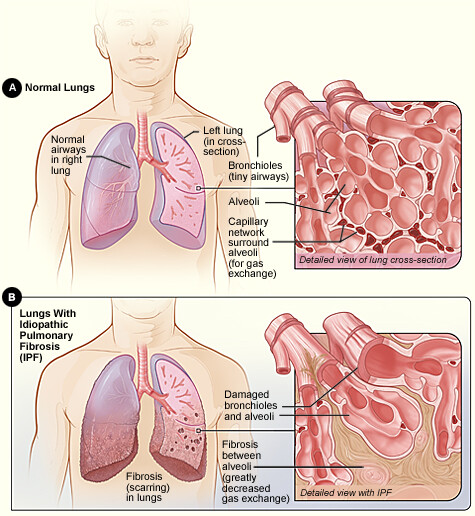
Pulmonary fibrosis
Results in scarring of the lung tissue that restricts the ability of the lung to fully expand with breathing decreasing lung function and leading to shortness of breath. Certain types of fibrosis can be caused by factors in the environment such as mold, being around birds, or exposure to certain chemicals or lung irritants. For many patients, with idiopathic pulmonary fibrosis, no cause can be found. As the lungs become more scarred, patients have worsening shortness of breath, decreased oxygen levels, and a chronic dry cough.
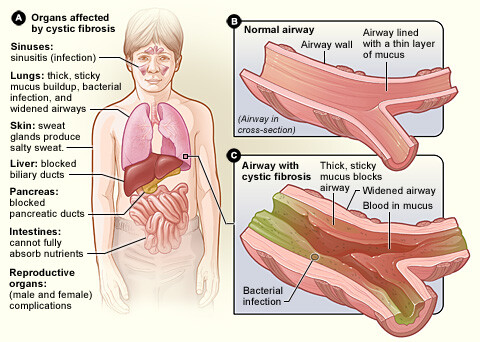
Cystic fibrosis (CF)
A disease that affects the cells that produce your body’s mucus, sweat, and digestive juices. It is an inherited disease, which means it can be passed only to children with parents who both have the CF gene. Some people may not experience symptoms until adolescence or adulthood, depending on the severity of the disease.
Normally, your body’s secreted fluids are thin and slippery, but in people with CF, a defective gene causes the secretions to become thick and sticky. The thicker secretions plug up tubes, ducts, and passageways, especially in the lungs and pancreas. CF can cause a persistent cough that produces thick mucus, repeated lung infections, inflamed nasal passages or a stuffy nose, poor weight gain and growth, and severe constipation.
Symptoms of CF may worsen as time passes, and recurrent infections can lead to bacteria resistant to antibiotics since the thick secretions are difficult for patients to clear from their airways.
Pulmonary hypertension
A form of high blood pressure that affects the arteries in your lungs and the right side of your heart. The disease develops when the arteries in your lungs, called pulmonary arteries, and capillaries become narrowed, blocked, or damaged. Pulmonary hypertension can cause an irregular heartbeat, racing pulse, dizziness, and shortness of breath, particularly when exercising. When severe, pulmonary hypertension can make it difficult for the right side of the heart to function well, leading to right heart failure. Patients with right heart failure can develop abdominal fluid and swelling of their legs.
The signs and symptoms depend on the underlying cause and the levels of oxygen and carbon dioxide in your bloodstream. COPD and emphysema can result in wheezing while patients with pulmonary fibrosis can have a chronic dry cough. Patients with cystic fibrosis can cough up thick mucus and have recurrent infections.
Low levels of oxygen in your blood due to end-stage lung disease can cause shortness of breath (feeling like you cannot get enough air in your lungs) and fatigue eventually limiting walking and other physical activity.
When severe, it can cause your skin, lips, and fingernails to have a bluish coloring or tint (cyanosis) requiring treatment with oxygen.
A high carbon dioxide level in your bloodstream can cause rapid breathing and confusion.
As a first step, your doctor will perform a physical exam and evaluate your overall health and any symptoms you are experiencing. In addition to the physical exam, your doctor will order a series of tests to evaluate your lungs including a chest X-ray, a chest CT scan, and pulmonary function tests.
While pulmonary fibrosis can be diagnosed on chest CT, this may require a special high-resolution chest CT. If this is not diagnostic, a lung biopsy using bronchoscopy (an endoscope passed through the nose or mouth or a surgical biopsy using thoracoscopy (small incisions in the chest wall) may be required. If pulmonary hypertension is suspected, an echocardiogram (ultrasound of the heart) or a right heart catheterization to directly measure the blood pressures in the pulmonary arteries may be performed.
Cystic fibrosis can be confirmed using a sweat test and genetic testing. An arterial blood gas may be obtained to determine the specific oxygen and carbon dioxide levels.
For more information on these tests, visit our common diagnostic tests page.
For all patients with end-stage lung disease, oxygen therapy should be considered when you have increasing shortness of breath and persistently decreased oxygen levels.
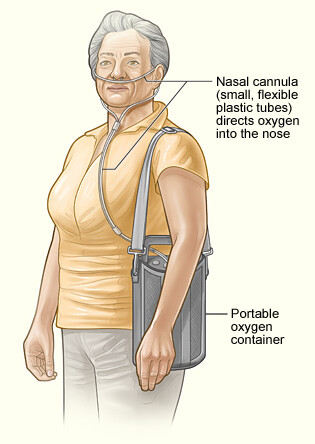
Oxygen is pushed into your lungs through a small plastic tube that fits into both nostrils or through a mask that fits over your nose and mouth. A portable oxygen tank can be used so patients can still walk and perform their daily activities.
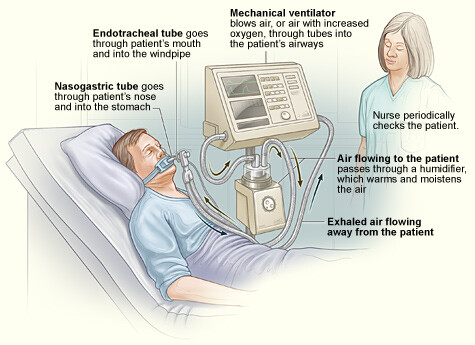
People who have severe lung disease and low oxygen levels even with oxygen treatment may need additional breathing support with a mechanical ventilator. This machine blows air into your lungs to help increase the oxygen level and to remove carbon dioxide when your lungs cannot do this on their own.
For patients with end-stage lung disease, lung transplant may be considered when other treatment options are no longer effective. Read our pages on adult lung transplantation and pediatric lung transplantation for more information on transplantation.
Patients with COPD and emphysema can be treated with:
Medications including inhalers that help dilate the airways and reduce inflammation.
Pulmonary rehabilitation programs can be beneficial in helping patients become more active and improving their overall function.
When medical therapy is not working, certain patients may be considered for lung volume reduction surgery (LVRS) to remove the most diseased portions of the lung giving the better parts of the lungs more room to work and allowing the diaphragm to function better. Studies have shown that LVRS only benefits a small subset of patients who have disease worse in part of the lung (usually worse in the upper portions of the lung) rather than emphysema throughout the lung. To be considered for LVRS, you would need to be evaluated by a thoracic surgeon and a pulmonologist at a specialized center that performs this procedure and would need to undergo additional testing to determine if you would be a good candidate.
Patients with COPD and emphysema can be treated with:
Medications including inhalers that help dilate the airways and reduce inflammation.
Pulmonary rehabilitation programs can be beneficial in helping patients become more active and improving their overall function.
When medical therapy is not working, certain patients may be considered for lung volume reduction surgery (LVRS) to remove the most diseased portions of the lung giving the better parts of the lungs more room to work and allowing the diaphragm to function better. Studies have shown that LVRS only benefits a small subset of patients who have disease worse in part of the lung (usually worse in the upper portions of the lung) rather than emphysema throughout the lung. To be considered for LVRS, you would need to be evaluated by a thoracic surgeon and a pulmonologist at a specialized center that performs this procedure and would need to undergo additional testing to determine if you would be a good candidate.
Medications that suppress the immune system may be helpful for certain types of pulmonary fibrosis. A lung biopsy may be required (as described above) to determine the specific type of fibrosis.
If a specific cause is found such as mold, being around birds, or exposure to chemicals, they should be removed from the patient’s home or work environment.
While there is no specific cure for idiopathic pulmonary fibrosis, newer medications may be useful in mild idiopathic pulmonary fibrosis in preventing further scarring and decline in pulmonary function. Whether you are a candidate for one of these medications should be discussed with your pulmonary doctor.
Medications that suppress the immune system may be helpful for certain types of pulmonary fibrosis. A lung biopsy may be required (as described above) to determine the specific type of fibrosis.
If a specific cause is found such as mold, being around birds, or exposure to chemicals, they should be removed from the patient’s home or work environment.
While there is no specific cure for idiopathic pulmonary fibrosis, newer medications may be useful in mild idiopathic pulmonary fibrosis in preventing further scarring and decline in pulmonary function. Whether you are a candidate for one of these medications should be discussed with your pulmonary doctor.
Patients with cystic fibrosis can often manage their disease using various therapies including:
Medications to help break up mucus and improve digestion (oral enzymes with meals).
Chest physical therapy involves pounding on your back and chest to help break up the mucus that clogs your airways. This can be done by a parent or family member who pounds on your back while you are lying on the floor. If this is too difficult or uncomfortable, you can be given a medical device to help break up the mucus such as vest that uses high-frequency vibrations to force the mucus in the direction of your upper airway so you can cough it up or a small, handheld device that vibrates when you forcefully exhale to help dislodge the mucus.
Antibiotics are used to treat infections and may need to be adjusted with recurrent infections if patients develop resistant bacteria.
Patients with cystic fibrosis can often manage their disease using various therapies including:
Medications to help break up mucus and improve digestion (oral enzymes with meals).
Chest physical therapy involves pounding on your back and chest to help break up the mucus that clogs your airways. This can be done by a parent or family member who pounds on your back while you are lying on the floor. If this is too difficult or uncomfortable, you can be given a medical device to help break up the mucus such as vest that uses high-frequency vibrations to force the mucus in the direction of your upper airway so you can cough it up or a small, handheld device that vibrates when you forcefully exhale to help dislodge the mucus.
Antibiotics are used to treat infections and may need to be adjusted with recurrent infections if patients develop resistant bacteria.
Primary pulmonary hypertension is not curable, but treatments are available to help decrease symptoms and improve quality of life. Medications are available that help to decrease the pulmonary blood pressures.
A cardiologist can help to determine whether you are a candidate for these medications.
Primary pulmonary hypertension is not curable, but treatments are available to help decrease symptoms and improve quality of life. Medications are available that help to decrease the pulmonary blood pressures.
A cardiologist can help to determine whether you are a candidate for these medications.
The outlook depends on the severity and type of underlying disease, how quickly treatment begins, and your overall health.
If your disease continues to worsen or if you are no longer able to manage your condition with therapies and medication alone, you may need to speak with your doctor about the possibility of meeting with a cardiothoracic surgeon to discuss a lung transplant.
See our pages on pediatric lung transplantation and adult lung transplantation for more information.
Reviewed by: Robbin G. Cohen, MD
July 2016
Previously reviewed by: Jules Lin, MD

