- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
Damaged or unhealthy lungs often have trouble exchanging oxygen and carbon dioxide, making it difficult for other organs to operate effectively. There are a variety of diseases that can damage your lungs including:
- Chronic obstructive pulmonary disease (COPD)/Emphysema
- Scarring of the lungs (pulmonary fibrosis)
- Cystic fibrosis
- Pulmonary hypertension
Read our page on End-Stage Lung Disease for more information on these diseases and other treatment options.
These lung diseases usually are treated initially with medications and eventually with supplemental oxygen. But when these treatments are no longer successfully controlling your breathing symptoms or when your lung function becomes life-threatening, your doctor might suggest a lung transplant.
Patients listed for transplant should meet the following general guidelines:
- End-stage lung disease that doesn’t respond to medical treatment
- No other significant medical problems
- No active infections outside of the lungs
- A life expectancy of less than 2 years due to lung disease
- Adequate functional status to recover from a lung transplant (based on how far you can walk in 6 minutes)
- Good support system
- No alcohol, narcotic, tobacco or recreational drug use for 6 months
Once you have been recommended for a lung transplant, you will meet with a transplant team that will perform an evaluation to determine if transplant will be a safe and effective treatment for your lung disease.
The transplant team will consist of a cardiothoracic surgeon, pulmonologist, nurses, social worker, and others, who all specialize in lung transplantation. Your evaluation likely will include:
- A physical examination
- Imaging studies, including a chest CT scan
- Blood tests
- Tests to check your heart and lung pressures and function
- Additional tests, such as a colonoscopy and a bone density scan, to confirm you do not have other serious medical conditions
- Tests and questions to ensure you are not using recreational drugs, alcohol, or tobacco
- A psychological evaluation
- Tissue typing (helps doctors know what donor lungs will match and decreases the chance that your body will reject the donated lungs)
Once the transplant team has finished the evaluation and you have been accepted as a transplant candidate, you will be placed on a nationwide transplant waiting list.
The amount of time you spend on the waiting list can vary from a few months to 2 to 3 years, and a number of factors determines your place on the waiting list, including:
- How sick you are (Lung Allocation Score)
- What lung disease you have
- Blood type
- Your size (to get the appropriate size donor lung)
- Overall medical condition
- Your panel of reactive antibodies (PRA) score (how likely you are to reject tissue from other people)
While you are on the list, your transplant center will provide you with a pager or cellphone, which it will use to notify you when a potential donor lung is available. You must keep this cellphone or pager charged and turned on at all times. When you are notified that a donor lung is available, you will be expected to travel to the hospital immediately to prepare for the transplant.
Not all patients who undergo evaluation are accepted as transplant candidates. You may be ineligible for lung transplant or become ineligible after you are listed if you:
- Are too sick to undergo the procedure (based on how far you can walk in 6 minutes)
- Continue to smoke or abuse alcohol or other drugs
- Have active hepatitis B, hepatitis C, or HIV
- Have had cancer within the past 5 years
- Have resistant infections that will likely affect the new lung
- Have severe disease of other organs (heart, liver, or kidney disease)
- Have inadequate family support
- Are severely obese
- Are severely malnourished
Before the operation can begin, you must undergo a final evaluation and blood work at the hospital. Once all of the final tests have been completed, you will be taken into the operating room (OR).
A single lung transplant usually takes 4 to 8 hours, while a double lung transplant can take from 6 to 12 hours to complete.
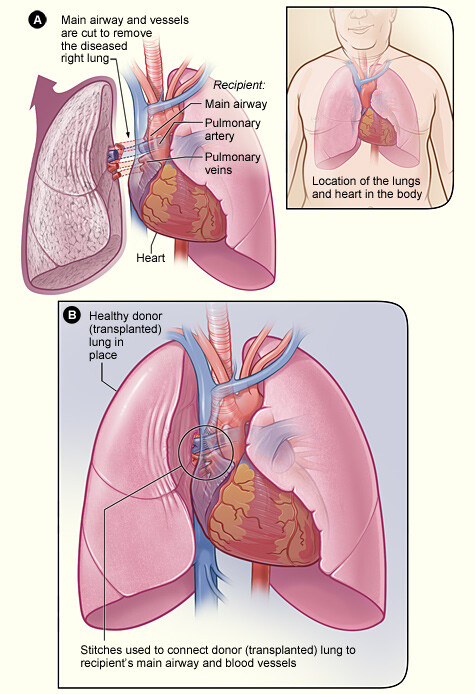
During the procedure, a cardiothoracic surgeon who specializes in transplantation will open your chest to remove your diseased lung or lungs, depending on your procedure. Once the diseased lung is removed, the surgeon will place the new lung in your chest and connect the main airway to that lung and the blood vessels between the lung and your heart.
If you are undergoing a double lung transplant, the surgeon will transplant one lung completely before transplanting the second.
You will be placed under general anesthesia during the procedure, and you also may be placed on a heart-lung machine during the operation. If needed, the machine temporarily takes over the function of your heart and lungs during surgery to maintain blood circulation through your body and the exchange of oxygen and carbon dioxide. After the surgery is completed, you will be taken off the heart-lung machine, and your heart and lungs will resume normal function.
For at least the first 24 to 48 hours, you will need to be in the intensive care unit (ICU) so doctors and nurses can monitor your condition carefully. Close follow-up is critical during the first few days after a transplant to ensure that you do not get an infection and that your lungs are working well.
The initial recovery period for lung transplantation is about 6 months. If you traveled a long distance for your surgery, your transplant team may ask you to stay close to the hospital for the first 3 months after you are discharged so they can better monitor your recovery.
The first year after your transplant is the most critical because this is when surgical complications, rejection, and infection pose the greatest risk.
The 1-year survival after lung transplant is 80-90%. The 3-year survival is 60-80%, and the 5-year survival is 50-60%. However, with improvements in post-transplant care, there are now patients who are surviving more than 20 years after their lung transplants.
After your initial recovery, you should expect to have regular checkups with your pulmonologist, and you may undergo regular bronchoscopies with lung biopsies to evaluate for any signs of rejection. You likely will have to take immunosuppressive medications (sometimes called antirejection medications) for the rest of your life. These medications help your body accept the new lungs and reduce the risk of transplant rejection. There can be side effects from these medications, however, so you will be required to schedule regular checkups with your doctor.
Maintaining an overall healthy lifestyle is important to keeping your new lungs healthy and extending the life of your transplant.
Smoking is not allowed, and your doctor likely will limit your intake of alcohol. Following a nutritious diet also can help you stay healthy.
Exercise is an important part of rehabilitation after your lung transplant and likely will begin quickly after your transplant, once you have recovered from the surgery and your incisions have healed. Speak with your doctor after your transplant to put together an exercise plan that you will be able to maintain.
Reviewed by Jules Lin, MD
May 2016