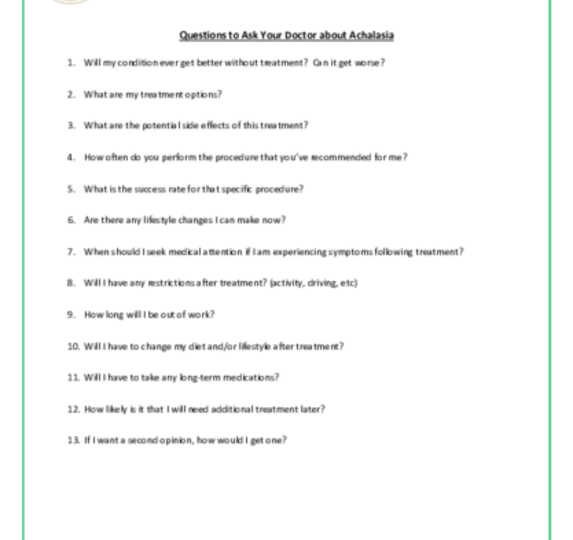
Achalasia and Esophageal Motility Disorders
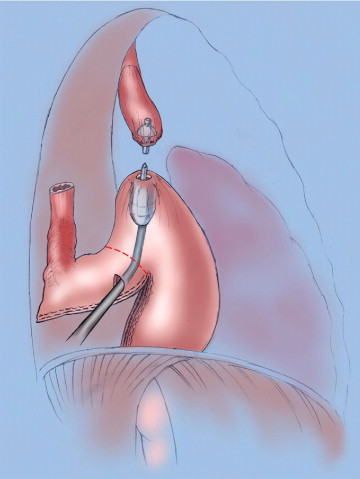
The esophagus (ĕ-sof´ah-gus) is the hollow, muscular tube that moves food and liquid from your mouth to your stomach. If the muscles in your esophagus don’t squeeze properly, it will be harder for the food and liquids to reach your stomach. This condition is known as an esophageal motility disorder. Esophageal motility disorders make it difficult for you to swallow, cause food to come back up into your mouth, and sometime cause chest pain.
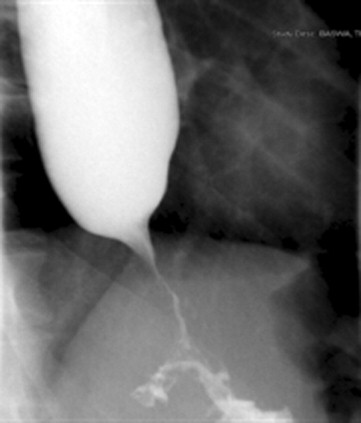
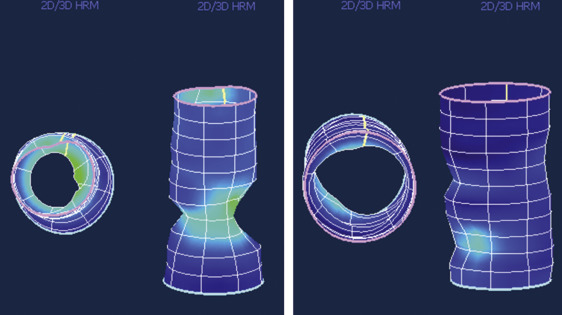
One type of esophageal motility disorder is achalasia (ak-uh-lā´-zhuh). Achalasia occurs when the nerves in the esophagus degenerate. As a result, the muscles in the esophagus stop working (no peristalsis), and the valve at the bottom of the esophagus doesn’t open. The condition is believed to affect 1-2 people in every 100,000, with about 3,000 new cases diagnosed each year in the United States.
Other less common dysmotility disorders include spastic esophageal motility disorder (nutcracker esophagus and diffuse esophageal spasm), inefficient esophageal motility disorder, and secondary esophageal motility disorders, which are related to other medical conditions like scleroderma, diabetes, and alcohol consumption.
Left untreated, achalasia can cause considerable weight loss, lung infections, and pneumonia.
It is important to remember that no treatment will cure achalasia, but all forms of treatment will help manage symptoms.