Mitral valve disease occurs when the mitral valve doesn’t work properly.
- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
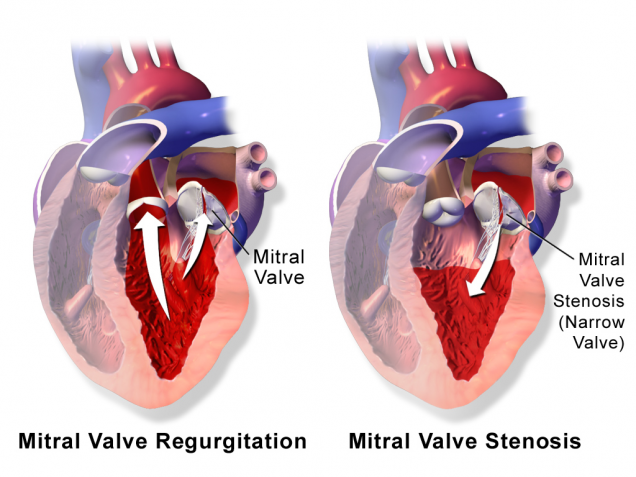
There are two main types of mitral valve disease:
- Stenosis – the valve does not open enough to allow sufficient blood flow. Usually this is the result of hardening (calcification) of the leaflets, which prevents their movement.
- Regurgitation – blood leaks backward out of the valve. Usually this is either the result of the leaflets being pulled apart so that blood leaks backward between them, or by damage to the valve structure.
Mitral valve stenosis is most commonly caused by inflammation from rheumatic fever, a disease that is related to strep infections; however, rheumatic fever is rare in the United States and other developed countries, so mitral valve stenosis is becoming less common.
Mitral valve regurgitation can develop slowly (chronic) or suddenly (acute). Chronic regurgitation can be caused by a number of diseases and conditions, including heart infection (endocarditis), high blood pressure, coronary artery disease, and mitral valve prolapse, in which the flaps bulge backwards when your heart contracts.
Acute mitral valve regurgitation is caused by a sudden rupture due to a heart attack, chest injury, or inflammation.
Some people may be born with mitral valve abnormalities (congenital).
A faulty or failing mitral valve may cause symptoms such as cough, shortness of breath, swollen feet or legs, chest pain, fatigue, and lightheadedness. Symptoms typically appear or worsen when your heart rate increases (such as during exercise) and may be triggered by an infection or pregnancy.
Your doctor can usually diagnose mitral valve disease based on your medical history, risk factors, a physical exam, and results from tests and procedures.
There is no one test that can diagnose mitral valve disease, so your doctor may recommend one or more of the following: electrocardiogram (EKG), echocardiogram (echo), chest x-ray, blood tests, and coronary angiography. For more information on these tests, visit the common diagnostic tests page.
A faulty mitral valve that is not causing symptoms may not need any treatment, and mild symptoms may be treated with medication. With more severe symptoms, surgery may be required.
Doctors will often repair the mitral valve when possible, but replacement is sometimes necessary.
Together with you and your medical team, your doctor will determine the best treatment option based on your symptoms and test results. You can print these sample questions to use as a basis for discussion with your doctor or a cardiothoracic surgeon.
You also can access the STS Risk Calculator, which can help calculate your risk of death or other complications from certain types of heart surgery. The results can help you and your doctor to determine the best course of treatment.
Medication cannot correct a faulty mitral valve, but it can help reduce symptoms. Potential medications include those that affect your blood pressure, heart rate, or the amount of extra fluid in your body.
Medication cannot correct a faulty mitral valve, but it can help reduce symptoms. Potential medications include those that affect your blood pressure, heart rate, or the amount of extra fluid in your body.
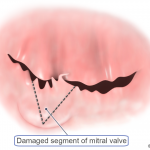
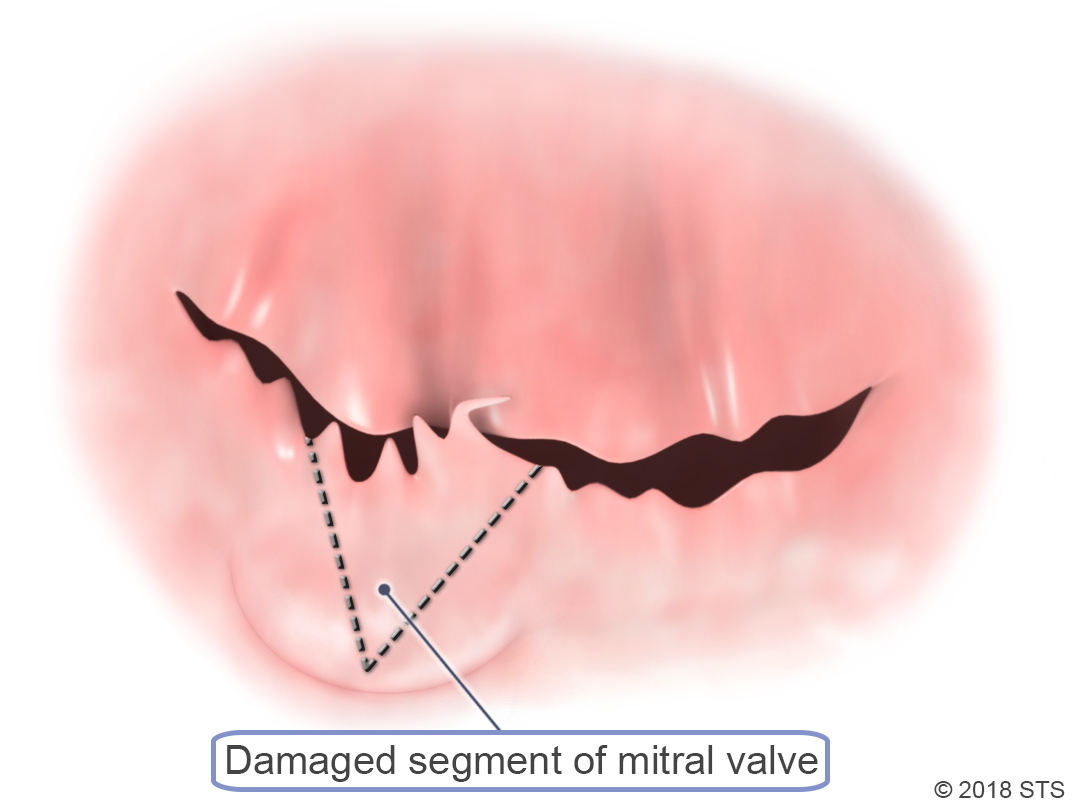
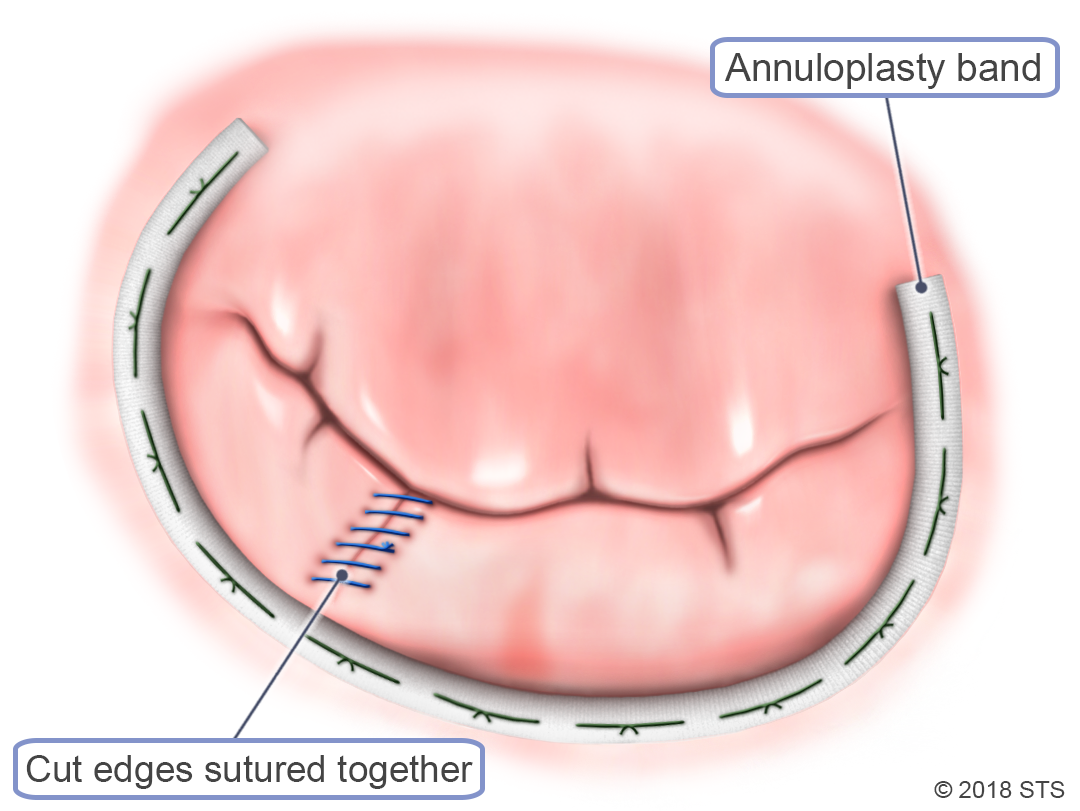
If your symptoms are more severe, your mitral valve may need to be repaired. A cardiothoracic surgeon can perform a surgical procedure to remove or reshape tissue, patch holes or tears in the valve, or separate flaps that have fused together.
There are two different surgical approaches that can be utilized: traditional or minimally invasive.
During traditional mitral valve surgery, the cardiothoracic surgeon makes a 6- to 8-inch long incision down the center of your sternum (breastbone) to open the chest, providing direct access to your heart.
In minimally invasive surgery, the surgeon makes a 2- to 4-inch, J-shaped incision that opens part of your chest. This can potentially reduce hospital stay.
Minimally invasive surgery is not appropriate for all patients, but your surgeon will review the recommended approach to surgery that is safest for you based on your individual symptoms and circumstances.
If your symptoms are more severe, your mitral valve may need to be repaired. A cardiothoracic surgeon can perform a surgical procedure to remove or reshape tissue, patch holes or tears in the valve, or separate flaps that have fused together.
There are two different surgical approaches that can be utilized: traditional or minimally invasive.
During traditional mitral valve surgery, the cardiothoracic surgeon makes a 6- to 8-inch long incision down the center of your sternum (breastbone) to open the chest, providing direct access to your heart.
In minimally invasive surgery, the surgeon makes a 2- to 4-inch, J-shaped incision that opens part of your chest. This can potentially reduce hospital stay.
Minimally invasive surgery is not appropriate for all patients, but your surgeon will review the recommended approach to surgery that is safest for you based on your individual symptoms and circumstances.
If the mitral valve is too damaged, it may need to be replaced. There are two options for mitral valve replacement—mechanical valves (metal) or biological valves (tissue).
The principal advantage of mechanical valves is their durability—they do not wear out; however, blood tends to clot on mechanical valves, so patients must take blood thinning medication (anticoagulants) for the rest of their lives. There is also a small risk of stroke due to blood clotting.
Biological valves usually are made from animal tissue. Biological valves are less likely to cause blood clots, but they also are less durable than mechanical valves and may need to be replaced in the future.
Like mitral valve repair, replacement can be done minimally invasively or with traditional open heart surgery.
Your medical team will discuss the advantages and disadvantages of both valve types with you prior to surgery.
If the mitral valve is too damaged, it may need to be replaced. There are two options for mitral valve replacement—mechanical valves (metal) or biological valves (tissue).
The principal advantage of mechanical valves is their durability—they do not wear out; however, blood tends to clot on mechanical valves, so patients must take blood thinning medication (anticoagulants) for the rest of their lives. There is also a small risk of stroke due to blood clotting.
Biological valves usually are made from animal tissue. Biological valves are less likely to cause blood clots, but they also are less durable than mechanical valves and may need to be replaced in the future.
Like mitral valve repair, replacement can be done minimally invasively or with traditional open heart surgery.
Your medical team will discuss the advantages and disadvantages of both valve types with you prior to surgery.
Immediately after surgery, you likely will have a tube in your throat so that your breathing can be assisted by a ventilator. The tube will be removed once you are able to breathe completely on your own. You likely will spend several days recovering in the hospital, although the total length of time depends on your overall health, as well as the specific procedure you underwent.
Once you’re home, it may be several weeks until you are able to go back to work, depending on your job. Everyday activities such as driving and lifting heavy objects may be restricted for a period of time. Blood thinning medication may be prescribed for 6 weeks to 3 months after surgery if you have a biological valve and for life if you have a mechanical valve.
After your wounds have healed, you should be able to get back to your normal activities. Always tell a doctor about your valve surgery before any medical procedure. This includes your dentist, as you may require preventative antibiotics when having dental work.
Reviewed by: Robbin G. Cohen, MD, with assistance from John Hallsten and Travis Schwartz
July 2016
Previously reviewed by: Emily A. Farkas, MD and Fernando Fleischman, MD