Extracorporeal membrane oxygenation (ECMO) is a technique that replaces the functions of failing lungs and/or the heart.
People with life-threatening but reversible heart or lung illnesses who have not responded to standard treatments may be candidates for ECMO. For example, ECMO may be used for severe lung damage from infection or shock after a massive heart attack. ECMO also can be used to support a failing heart after heart surgery. ECMO can provide support for days to weeks while doctors treat the underlying illness.
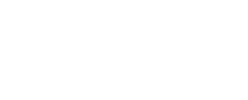
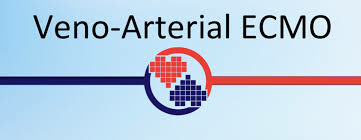
Extracorporeal means that the blood circulates outside of the body through a tube or catheter with the help of a machine. Membrane oxygenation, referred to as the “artificial lungs,” is a special part of the machine that puts oxygen into the blood and takes out carbon dioxide, just like the lungs do. ECMO also is known as extracorporeal life support (ECLS), and the ECMO machine often is referred to as a type of heart-lung machine.
During ECMO treatment, the heart continues to beat, but its work is made easier because the ECMO machine does much of the pumping. The goal of ECMO is to ensure that the body has enough blood flow and oxygen by temporarily managing the workload of the heart and lungs. ECMO provides time for the body to rest and recover, but it will not directly heal the heart or lungs.
ECMO was initially developed and used for babies in critical condition whose lungs were not functioning, but it is now being used more for adults. According to the Extracorporeal Life Support Organization (ELSO), more than 100,000 patients have been on ECMO over the past several decades.