News & Trending Topics
Allowing select patients to self-manage blood thinners following heart valve surgery may lead to a lower risk of major complications, according to an article posted online by The Annals of Thoracic Surgery.
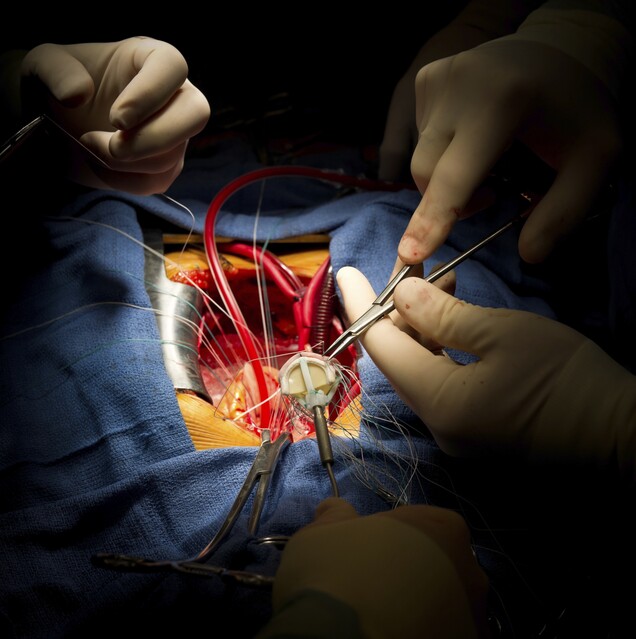
Two kinds of heart valves are available for patients undergoing valve replacement surgery. Biological valves are made from animal tissue and have the potential to wear out, especially in younger patients. Mechanical valves are made of metal and do not wear out, but require anticoagulation therapy (blood thinners) to help prevent blood clots, which could lead to strokes. The only anticoagulants currently available to these patients are vitamin K antagonists, such as warfarin or phenprocoumon.
“Oral anticoagulation therapy is usually monitored by laboratory analysis of the patient’s blood, which health care providers use to determine the appropriate dosage of medication,” said Thomas Decker Christensen, MD, PhD, from Aarhus University Hospital in Denmark, who led the study. “We believe that allowing patients to have more control over their own treatment can improve the standard of care in this patient group.”
Dr. Christensen and colleagues evaluated the use of patient self-management of anticoagulation therapy at two hospitals in Denmark between 1996 and 2012 and compared it to the standard management. Their study included 615 patients with mechanical heart valves who self-managed treatment and 3,075 control patients (a 5:1 ratio) who received standard treatment management following valve surgery.
Patients were required to attend an educational program containing a minimum of three teaching lessons in order to be eligible for self-management. Over a period of 27 weeks following the educational training, patients gradually became self-managed.
“Once patients were approved for self-management, they were allowed to continue as such but could contact the treatment center with questions or concerns,” said Dr. Christensen. “Patients were provided with a portable coagulometer, which they used to analyze medication levels and monitor dosage. Blood levels were measured and tracked weekly.”
Patients compared their own measurements against the International Normalized Ratio, a number that explains how quickly blood clots. Based on this ratio, patients adjusted their dosage levels according to what they had been taught in the educational training.
Researchers observed low rates of adverse events among patients who transitioned to self-management. At 1 year after treatment, the risk of major bleeding and thromboembolism (a blood clot that moves through the bloodstream and blocks another vessel) were similar in both treatment groups. After 5 years, however, patients who self-managed their anticoagulants had a lower risk of all-cause mortality compared to standard management patients.
“There are several reasons that patients who self-manage treatment have better outcomes than those who follow standard management,” explained Dr. Christensen. “Self-management patients receive more detailed information about oral anticoagulation therapy; they also learn more about the influence that diet, infectious diseases, alcohol, and other drug interactions can have on their treatment than do patients receiving standard management.”
He added that he hopes this study will have an impact on the management and care of heart valve patients, “We believe that the majority of patients who have a mechanical heart valve inserted during surgery should be able to manage their oral anticoagulant therapy, and recommend this as the standard treatment approach for these patients.”