- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
February 17, 2017

The earliest version of minimally invasive chest surgery (thoracic surgery) occurred more than 100 years ago. In 1913, instead of relying on a large chest incision, a thoracic surgeon inserted a small scope into the chest of a tuberculosis patient and removed scar tissue from around the lung. This “thoracoscopic” surgery was performed using a cystoscope, something normally used by urologists to visualize the inside of the bladder. One can only imagine the view inside the chest with the only illumination being that of candlelight!
Enthusiasm for thoracoscopies waned after the discovery of Streptomycin (an antibiotic) as medical treatment for tuberculosis. But that changed in the 1990s, aided largely by advances in surgical instrumentation, cameras, and video monitoring. Of these, the most significant was video monitoring, which allowed for magnification and eliminated the need for the surgeon to peer down the barrel of a poorly illuminated scope. Hence the new term “Video-Assisted Thoracoscopic Surgery” (VATS) was born. Today, more than 70% of all cases performed in busy thoracic surgical practices use some version of minimally invasive surgical techniques.
Thoracic Surgical Approaches
There are inconsistencies by which the term “minimally invasive” surgery is applied even today. In general, minimally invasive surgery of all types uses incisions that are considerably smaller than traditional incisions but may vary in number. In the case of thoracic surgery, we consider those surgical techniques that avoid either cutting or spreading of the ribs to be minimally invasive. Avoidance of the latter is important since trauma to the ribs is a major contributor to post-operative pain.
Traditional Thoracic Incisions
The most common incisions for traditional thoracic surgery are the thoracotomy and median sternotomy. Both are often referred to as “open” surgery. Thoracotomy involves an 8-12 inch incision on the side and back of the chest. A portion of one or more ribs is either removed or surgically cut in order to accommodate traditional surgical instruments and for complete visualization of the chest cavity. A sternotomy is a vertical incision down the front of the chest and involves surgically cutting the sternum (breastbone). The sternum is then re-closed at the end of the surgical procedure. The vast majority of all thoracic surgeries can be accomplished via one of these approaches. They are some of the oldest procedures with excellent long-term outcomes and are the mainstay of any thoracic surgeon’s preferred techniques.
Video-Assisted Thoracoscopic Surgery (VATS)
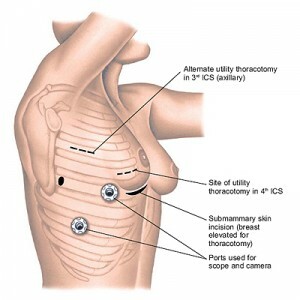
VATS procedures are performed using small incisions (called ports), a lighted camera, and a high-definition video monitor. It may involve a single port or multiple ports. The camera transmits images of the operative area to a video monitor, guiding the surgeon as he or she operates. The thoracoscope provides an excellent view of the entire chest without the need for spreading or cutting ribs. Surgical trauma is further minimized by use of specially designed instruments.
Robotic-Assisted Thoracoscopic Surgery
The newest addition to the options for minimally invasive techniques is that of the surgical robot. Robotic-assisted thoracoscopic surgery (RATS) is similar to VATS in that it uses several small ports and a lighted camera with video monitoring. There are several key differences, however. The chief difference among them is that RATS requires the use of a robotic operating system. In a RATS procedure, the primary surgeon is not at the patient’s bedside, rather he or she is seated at a nearby console in the operating room. The surgeon controls the robot’s movements operating from the console and a surgical assistant or second surgeon is positioned at the operating table to assist with changing instruments and other aspects of the procedure. Two strengths of robotic systems are the 3D technology allowing for visualization in greater detail and the small instrument tips that allow surgeons to work more easily in tight places.

Use of Minimally Invasive Techniques in Thoracic Surgery
The progression from maximally to minimally invasive techniques in thoracic surgery is reflected in the overall trend of more surgeons who are trained in these techniques and thus incorporating them into their practice. Initial slow enthusiasm was linked to skepticism that minimally invasive surgery might compromise cancer outcomes or functional outcomes at the expense of the aesthetics of smaller incisions. Fortunately, research comparing surgical techniques have largely refuted these concerns and support the reported benefits of minimally invasive techniques.
Benefits of minimally invasive surgery
- Less post-operative pain
- Reduced risk of Infection
- Shorter hospital stays
- More rapid return to normal activities
- Less scarring
- Faster initiation of chemotherapy following surgery
- Better tolerance of chemotherapy following surgery
At the same time, the conditions for which minimally invasive techniques are used have also broadened. Historically, only minor procedures were performed using minimally invasive surgery, such as lung biopsy or drainage of the pleural space. Now, surgeons are routinely performing more complex procedures, including removal of an entire lung, esophageal resections for cancer, and large locally aggressive tumors traditionally reserved for thoracotomy. Additionally, even more techniques are being used that include combination or hybrid procedures, such as in the case of combined chest wall resection.
Common procedures done using minimally invasive techniques
- Lung cancer operations/lung resections
- Esophageal operations
- Biopsies of pleura or lungs
- Lobectomy and mediastinal lymph node dissection for lung cancer
- Wedge resection for solitary pulmonary nodules
- Wedge resection for pulmonary metastases
- Pneumonectomy for lung cancer
- Esophageal mobilization for esophageal cancer
- Thymectomy for myasthenia gravis
- Decortication for empyema (infection within the pleural space)
- Lung volume reduction surgery for emphysema
- Talc pleurodesis for recurrent benign or malignant pleural effusions
- Insertion of PleureX catheters for recurrent effusions
- Bleb resection and mechanical pleurodesis for recurrent pneumothoraces (collapsed lungs)
- Thoracic sympathectomy for hyperhidrosis (excessive sweating)
- First rib resection for thoracic outlet syndrome
- Heller myotomy for achalasia
How do I know what surgical approach is right for me?
Although the indications for minimally invasive thoracic procedures continue to expand, clear indications for open surgery remain. Many variables factor into the decision of one surgical approach over another including patient characteristics such as the medical condition of the patient, prior operations, other medical problems, procedure required, and patient anatomy.
Common conditions that may NOT be amenable to minimally invasive techniques:
- Previous open chest surgery
- Prior radiation to the chest
- History of pulmonary infections
- Prior coronary artery bypass graft surgery (CABG)
My goal in choosing between operative approaches is to achieve the necessary diagnostic and therapeutic outcomes for each patient while ensuring safety and a rapid recovery. Surgeon experience is paramount. Not all surgeons are experienced in advanced minimally invasive techniques. It is critical to finding a surgeon who you are comfortable with and who is experienced with several techniques so that you are confident in knowing that the best procedure for you is the one being offered and that it can be performed safely. At the end of the day, an expertly performed open surgery is still superior to a poorly performed minimally invasive one.
The opinions expressed in this article are those of the author and do not necessarily reflect the views of The Society of Thoracic Surgeons.

