- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
September 28, 2016

We are in a new era of lung cancer screening. Patients at risk for lung cancer can have similar access to early detection that patients with other cancers have had for decades.
This is important because lung cancer is the second most common cause of death in the United States, exceeded only by cardiovascular disease. (In fact, cardiothoracic surgeons are key specialists for both of the top two diseases in the US.)
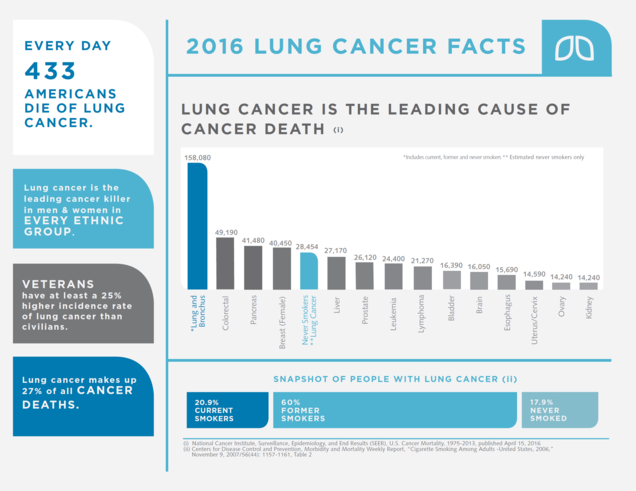
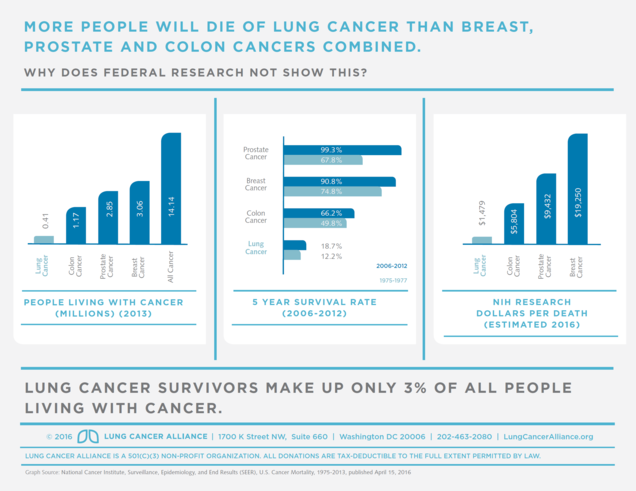
An astounding 158,000 Americans will die this year of lung cancer, a number that some have put into context by noting that it is the equivalent of a 747 plane crash occurring every day. More people die of lung cancer than breast, colon, prostate, and pancreas cancers combined, and it is the 5th most common cause of cancer death in never smokers.
Promising data about the use of low-dose computed tomography (LDCT) led to a very large research study in the United States called the National Lung Screening Trial (NLST). The NLST randomized more than 53,000 patients at high risk of lung cancer (ages 55-74 and at least a 30 pack-year smoking history) to low-dose CT versus just a chest x-ray. Those being screened with LDCT had a 20% decreased mortality from lung cancer—an enormous impact in the world of early cancer detection—and a greater impact than either mammography for breast cancer or colonoscopy for colon cancer. This study was published in The New England Journal of Medicine in 2011, and, at the end of 2013, the United States Preventive Services Task Force (USPSTF) updated its lung cancer screening recommendations.
Previously, the USPSTF had recommended AGAINST lung cancer screening. With the update in 2013, it recommended—for the first time—screening for patients at high risk of lung cancer. This is especially important because under the Affordable Care Act (“Obamacare”), recommendations from the USPSTF require insurance coverage of lung cancer screening as a preventive service, meaning that there is no associated co-pay for insured patients.
One irony in this decision was that Medicare makes independent decisions about coverage of services for Medicare beneficiaries and is not bound by USPSTF recommendations. And with 70% of lung cancer patients covered by Medicare, a majority of patients would still not have access to screening. Fortunately, experts at Medicare also evaluated the important new data from the NLST and approved lung cancer screening for Medicare beneficiaries on February 5, 2015.
For the first time, Americans at risk of dying from our most serious cancer have insurance coverage and widespread access for screening and early detection, offering new promise for improving survival rates in lung cancer like we have achieved in other cancers over recent decades.
As many as 12,000 – 15,000 lives can be saved each year through lung cancer screening programs.
Who Is Approved for Lung Cancer Screening?
There are some minor variations in who is approved and recommended to undergo lung cancer screening with low-dose CT. The Medicare coverage extends to the following patients who are considered “high risk” for lung cancer:
- Age 55-77
- Smoking history >30 pack-years (a “pack-year” equals the number of packs smoked per day multiplied by the number of years, e.g., 1 pack per day for 30 years = 30 pack-years)
- For those who have stopped smoking, once it has been 15 years since they quit, they would be ineligible for further screening under Medicare regulations.
It is important to note that non-smokers, those with a minimal smoking history or younger individuals, are at a very low risk of lung cancer, and it is not appropriate to undergo lung cancer screening. For those at a lower risk, the potential harms of screening (radiation exposure, unnecessary testing, and possible invasive procedures) outweigh the benefits and are discouraged. On the other hand, some expert groups like the National Comprehensive Cancer Network (NCCN) recommend that screening be considered for a broader group of patients than those covered in current Medicare policy. Fortunately, the NCCN also creates patient education materials about lung cancer screening.
Other medical societies and organizations have developed online educational materials and risk calculators that allow one to learn about individual risks of lung cancer. Some of those that are particularly useful for patients are:
Information on these sites can help you decide if you should consider lung cancer screening, and give you information on how to discuss this with you doctor.
Importance of Early Detection
One factor that is especially troubling for physicians and other health professionals caring for lung cancer patients is the gap between early diagnosis in lung cancer patients compared with early diagnosis in other common cancers like breast, prostate, and colon cancer.
Detecting cancer at an early stage, before it has spread, provides the best opportunity for successful treatment and cancer survival.
While other common cancers have benefited from programs of screening that have substantially improved rates of early diagnosis and an improvement in cancer survival over the past 30-40 years, patients at risk for lung cancer have not had access to lung cancer screening. Therefore, the majority of patients diagnosed with lung cancer already have spread of disease at the time of diagnosis, and the chance for cure is very small.
There is also a serious gap in research funding in lung cancer, compared to other major cancers, which may contribute to the lower rates of early diagnosis or improved cancer survival in lung cancer patients. Since lung cancer disproportionately impacts individuals who are older, lower socio-economic status, and minorities, one could worry that this lack of research focus or federal approval of lung cancer screening represents unfair disparities within the United States health care system, perhaps magnified by the stigma placed on smokers of being at fault for their own disease.
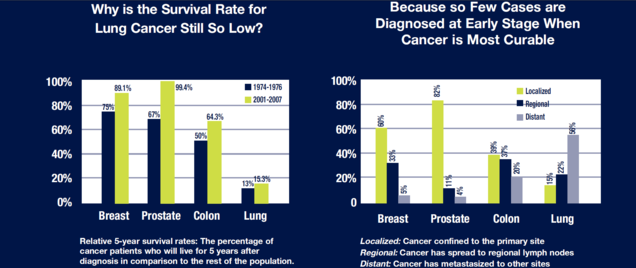
In spite of these depressing statistics, however, it is an exciting new era! Lung cancer screening allows early detection of lung cancer and the best opportunity for cure. This advance in cancer care provides one of the biggest potential impacts in decreasing death from cancer in a generation. Combined with efforts in smoking cessation, lung cancer screening is a step towards making lung cancer…history, a disease of the past.
The opinions expressed in this article are those of the author and do not necessarily reflect the views of The Society of Thoracic Surgeons.

