- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
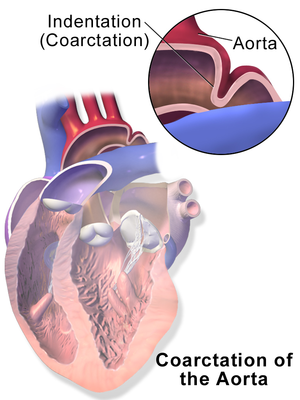
Coarctation of the aorta often occurs along with other heart defects. Treatment usually is successful, but careful follow-up during infancy and throughout adulthood is always recommended.
The US Centers for Disease Control and Prevention (CDC) estimates that 4 out of every 10,000 babies are born with coarctation of the aorta.
Congenital heart defects, such as coarctation of the aorta, are the result of problems that occurred early in the heart’s development. The defect forms while your baby’s heart is developing in the womb, but, like most congenital heart defects, there is no known cause.
In rare cases, coarctation of the aorta can develop later in life due to traumatic injury.
Severe hardening of the arteries (atherosclerosis) or a condition causing inflamed arteries (Takayasu’s arteritis) also may cause narrowing of the aorta, similar to a coarctation.
Coarctation of the aorta usually occurs in a spot beyond where the blood vessels branch off to the upper body. This often leads to high blood pressure in the arms, but low blood pressure in the legs and ankles. The coarctation often is near the insertion of the ductus arteriosis that closes after birth and becomes a ligament in the first year of life. One theory is that ductal tissue invades the wall of the aorta in patients who develop coarctation of the aorta.
You or your child may be more likely to have aortic coarctation if certain heart conditions exist, including:
- Bicuspid aortic valve
- Patent ductus arteriosus
- Holes in the wall between the left and right sides of the heart (septal defects)
- Aortic valve stenosis (to small an opening) or regurgitation (leaking)
- Mitral valve stenosis (to small an opening) or regurgitation (leaking)
- Turner syndrome
Symptoms depend on the degree of narrowing. Children with severe narrowing of the aorta most often show signs and symptoms early in life, while mild cases may not be diagnosed until adulthood. Left untreated, aortic coarctation in babies may lead to heart failure and death.
Signs and symptoms of severe coarctation of the aorta include:
- Irritability
- Heavy sweating
- Difficulty breathing
- Feeding difficulties
- Pale skin
In some infants, having difficulty feeding can increase the risk of developing other conditions, including necrotizing enterocolitis, a serious intestinal disease that happens when tissue in the small or large intestine is injured or begins to die off.
If signs or symptoms appear later in life, the most common sign is high blood pressure (hypertension). Other symptoms may include:
- Heart murmur
- Shortness of breath, especially during exercise
- Headache
- Muscle weakness
- Leg cramps or cold feet
- Nosebleeds
During a routine physical exam, a doctor should check the blood pressure and pulse in the arms and legs. Symptoms that your doctor may be able to find during this exam include:
- Weaker pulse in the groin area or feet than in the arms or neck
- Weaker blood pressure in your baby’s legs than in his/her arms
- A harsh-sounding heart murmur that can be heard from the back
Coarctation of the aorta is usually confirmed with an echocardiogram (echo). Occasionally other tests may be ordered, such as chest x-ray, computed tomography (CT) scan, electrocardiogram (EKG), pulse oximetry, cardiac catheterization, or magnetic resonance imaging (MRI).

For more information on these tests, visit our common diagnostic tests page.
Surgery, performed by a pediatric/congenital heart surgeon (cardiothoracic surgeon), is most often required to fix your child’s aorta, but catheter-based interventions also may be an option for some children. Most symptomatic newborns will have surgery very shortly after they are born. Children diagnosed when they are older also will need surgery, but because the symptoms are usually less severe, more time can be taken to plan for surgery.
Complications from coarctation of the aorta, if not treated, include:
- Narrowing of the aortic valve (aortic stenosis)
- High blood pressure
- Stroke
- Enlargement in a section of the wall of the aorta (aneurysm)
- Aortic rupture or tear (dissection)
- Premature coronary artery disease — narrowing of the blood vessels that supply the heart
- Heart failure
- A weakened or bulging artery in the brain (brain aneurysm) or bleeding in the brain (hemorrhage)
Be sure to speak with your child’s doctor about what procedure is right for him or her and to get more information on what you should expect during and after surgery. You can print these sample questions to use as a basis for discussion with the doctor.
Expected outcomes: The Society of Thoracic Surgeons (STS) Congenital Heart Surgery Database shows an expected outcome of 1% mortality for isolated coarctation of the aorta. Outcomes will vary across different programs. It is appropriate to inquire about the outcomes of a surgical group or surgeon during your consultation.
Depending on the location and extent of the coarctation, your child’s surgeon can approach it from the front of the chest (sternotomy) or from the left side of the chest (thoracotomy). Surgical techniques to repair aortic coarctation include:
Resection with end-to-end or extended end-to-end anastomosis – Removes the narrowed segment of the aorta (resection) and connects the two ends of the aorta (anastomosis)
Patch aortoplasty – Cuts across the constricted area of the aorta and then attaches a patch of synthetic material or a portion of the blood vessel that delivers blood to your left arm (left subclavian artery) to widen the blood vessel
Resection and interposition graft repair – Usually undertaken in older children and adults with coarctation - removes the narrowed segment of the aorta (resection). Then attaches a synthetic tube (graft) between the cut ends of the aorta
Depending on the location and extent of the coarctation, your child’s surgeon can approach it from the front of the chest (sternotomy) or from the left side of the chest (thoracotomy). Surgical techniques to repair aortic coarctation include:
Resection with end-to-end or extended end-to-end anastomosis – Removes the narrowed segment of the aorta (resection) and connects the two ends of the aorta (anastomosis)
Patch aortoplasty – Cuts across the constricted area of the aorta and then attaches a patch of synthetic material or a portion of the blood vessel that delivers blood to your left arm (left subclavian artery) to widen the blood vessel
Resection and interposition graft repair – Usually undertaken in older children and adults with coarctation - removes the narrowed segment of the aorta (resection). Then attaches a synthetic tube (graft) between the cut ends of the aorta
Percutaneous catheter-based intervention (sometimes called balloon angioplasty) also may be an option for treating your child’s coarctation. This procedure involves a thin flexible tube (catheter) that is inserted into your child’s artery through the groin and is threaded up through the blood vessels to the heart. An uninflated balloon is placed through the opening of the narrowed aorta. When the balloon is inflated, the aorta widens and blood flows more easily. The heart specialist may elect to leave a metal stent in the area of narrowing which will keep the aorta open after the balloon is deflated.
Percutaneous catheter-based intervention (sometimes called balloon angioplasty) also may be an option for treating your child’s coarctation. This procedure involves a thin flexible tube (catheter) that is inserted into your child’s artery through the groin and is threaded up through the blood vessels to the heart. An uninflated balloon is placed through the opening of the narrowed aorta. When the balloon is inflated, the aorta widens and blood flows more easily. The heart specialist may elect to leave a metal stent in the area of narrowing which will keep the aorta open after the balloon is deflated.
Care will be taken when re-introducing feeds, especially in cases of tight coarctation or a child that presents in shock. Hospital length of stay will vary depending on age and severity of the defect.
Your child will continue to be followed by a heart specialist.
The most common long-term complication of coarctation of the aorta is high blood pressure. Although blood pressure usually falls after the defect has been repaired, it may still remain higher than normal.
High blood pressure could result in the long-term use of medication, but be sure to speak with your child’s heart specialist about the need for continued medication.
In some cases, the portion of the aorta that was repaired can re-narrow, possibly even years after treatment. This often can be corrected by percutaneous intervention, but may require additional surgery. Rarely, the segment of the aorta that has been repaired can become weak and bulge (aortic aneurysm) and are at risk of rupture.
Reviewed by: Lauren Kane, MD
December 2017