Pleural Diseases
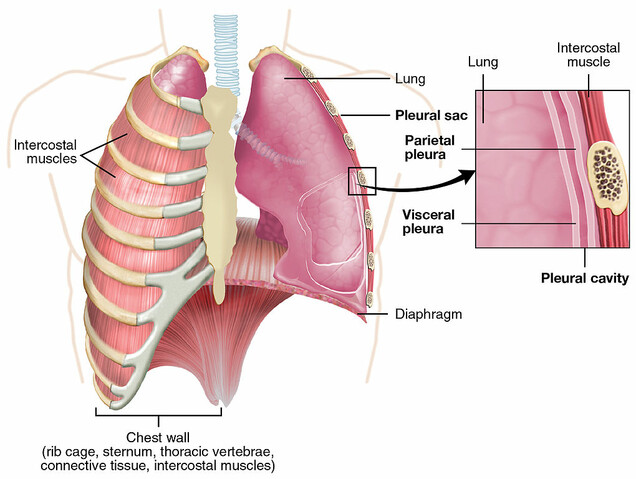
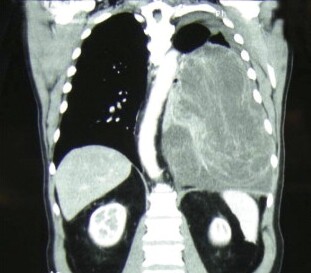
The pleura (ploor´-uh) is the membrane that lines your chest (thoracic) cavity and covers your lungs. The layers of your pleura contain a small amount of fluid that acts as a lubricant as you breathe in and out. The space between the layers is called the pleural cavity.
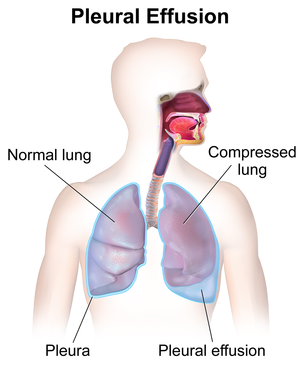
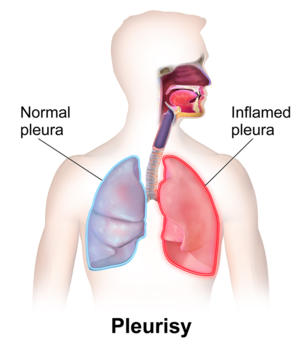
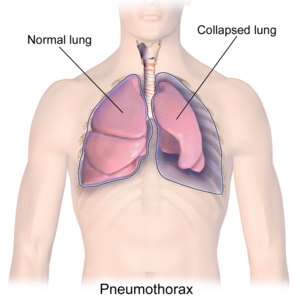
Pleural diseases include pleural effusion, pleurisy, pneumothorax, hemothorax, and pleural tumors.
Treatment for mechanical problems (fluid, air, or blood) focuses mainly on removing the fluid, air, or blood from the pleural space, relieving the symptoms, and treating the underlying condition.