Transposition of the Great Arteries
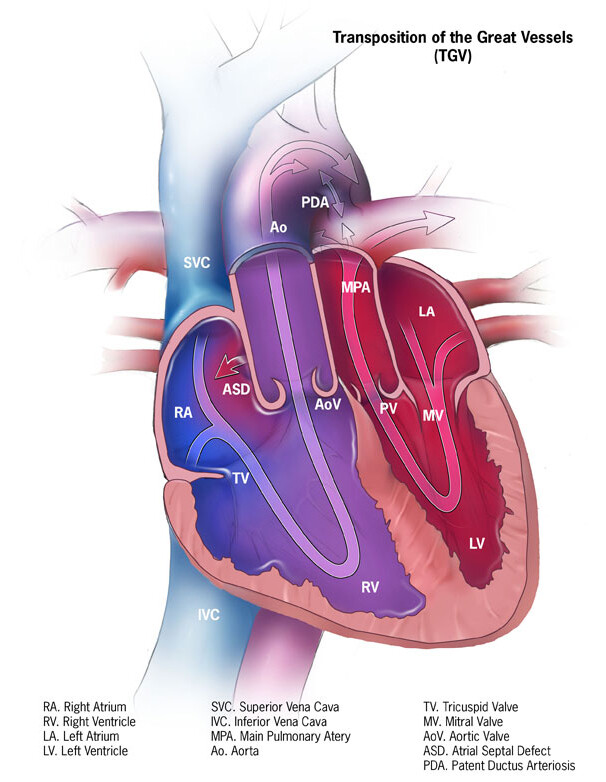
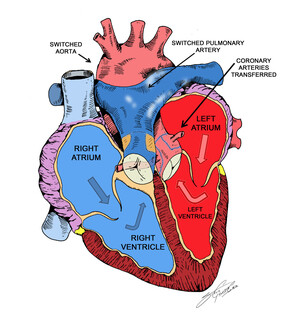
Transposition of the great arteries (TGA) is a rare but serious congenital (present at birth) heart defect, in which the two main arteries leaving the heart are reversed (transposed).
Normally, the aorta leaves the left ventricle carrying oxygen-rich (red) blood to the body, and the pulmonary artery leaves the right ventricle carrying oxygen-poor (blue) blood to the lungs to get oxygen. The reversal in TGA changes the way blood circulates through the body, causing a shortage of oxygen in the blood leaving the heart going to the rest of the body.
According to the National Heart, Lung, and Blood Institute (NHLBI), TGA affects roughly 5 out of every 10,000 babies. The defect is found more frequently in Caucasians. Untreated, more than 50% of infants with transposition will die in the first month of life, 90 % in the first year.
TGA can be diagnosed during pregnancy with ultrasound or soon after birth.
Babies who have surgery to repair TGA usually do well. More than 90% survive to adulthood and live active, healthy, and productive lives.