- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
The heart beats through its own electrical conduction system that not only coordinates squeezing of the heart chambers, but also determines how fast or slow the heart beats. A normal heart beats in a regular pattern of 60 to 100 times per minute (sinus rhythm).
Millions of people worldwide are affected by cardiac rhythm disturbances. In the United States, an estimated 1 in 18 people have some sort of cardiac rhythm disturbance, according to government statistics. The risk for these disturbances increases with age and certain specific and severe types could lead to sudden cardiac death. The American Heart Association estimates that 180,000 to 450,000 people die in the US annually from sudden cardiac death.
The main types of heart rhythm disturbances include:
- Tachycardia: A fast heart rhythm (more than 100 beats per minute)
- Bradycardia: A slow heart rhythm (fewer than 60 beats per minute)
- Supraventricular arrhythmias: Abnormal rhythms that begin in the heart’s upper chambers (atria)
- Ventricular arrhythmias: Arrhythmias that begin in the heart’s lower chambers (ventricles)
- Bradyarrhythmias: Slow heart rhythms that usually are caused by a disease in the heart’s conduction system
Some of the above categories of cardiac rhythm disturbances also can have subtypes:
SUPRAVENTRICULAR ARRHYTHMIAS
- Atrial Fibrillation (Afib) is the most common type of cardiac rhythm disturbance. It is characterized by a fast, irregular rhythm in which single muscle fibers in your heart twitch or contract in a disorganized way. Afib can cause blood to pool in the upper chambers of your heart, which can lead to blood clots. This can increase the risk of stroke as compared to someone without atrial fibrillation.
- Supraventricular Tachycardia (SVT) is a rapid but regular heartbeat that occurs when the electrical signals in your heart’s upper chambers fire abnormally and interfere with your heart’s pacemaking ability. The faster beats from the atria speed up your heart rate.
- Wolff-Parkinson-White Syndrome is a group of congenital (present from birth) heart defects that are caused by extra muscle pathways between the atria and the ventricles. The extra pathways cause your heart’s electrical signals to be disrupted because it takes too long for your heart to receive them.
VENTRICULAR ARRHYTHMIAS
- Ventricular Tachycardia occurs when the pacemaking role of your heart is taken over by an area of the heart that typically is not involved in the process. This causes your heart’s electrical signals to be sent down a different path than is usual, which can create an irregular heartbeat.
- Ventricular Fibrillation (Vfib) is one of the most serious cardiac rhythm disturbances. It is an irregular, uncontrolled heartbeat that occurs when your heart receives impulses from different locations at the same time, telling it to beat. This creates an erratic, fast heartbeat that can only be controlled through immediate medical attention.
- Premature Ventricular Contractions occur when your ventricle contracts too soon, which takes it out of sequence with your normal heartbeat. These disturbances often are not serious and do not always require treatment.
Causes of Cardiac Rhythm Disturbances
Disturbances in your heart rhythm can be caused by many different environmental factors, as well as other health problems.
Environmental causes can include:
- Smoking
- Alcohol abuse
- Use of some drugs (such as cocaine or amphetamines)
- Abuse of certain prescription or over-the-counter medicines
Too much caffeine or nicotine also can sometimes lead to arrhythmia.
High blood pressure, diabetes, or the presence of too much stress hormone (cortisol) in your bloodstream can lead to an arrhythmia because these conditions cause your heart to work too hard.
Other health conditions that can lead to arrhythmia in some people include:
- Heart attack
- Coronary heart disease
- Heart failure
- Overactive or underactive thyroid gland (too much or too little thyroid hormone produced)
- Rheumatic heart disease
Certain congenital heart defects (present at birth) can cause arrhythmias. See Congenital Heart Defects for more information on these conditions.
Symptoms of Cardiac Rhythm Disturbances
Symptoms of cardiac rhythm disturbances can vary, depending on the type and severity. If you have an arrhythmia, you may feel a fluttering sensation in your chest, such as a palpitation. You also may feel “extra” heart beats as if your heart is beating more often than it should.
If you have tachycardia, you also may feel like your heart is racing or beating very fast. Bradycardia and bradyarrhythmias cause your heart to beat more slowly so you may feel sluggish or like your heart is beating very slowly. You also may feel as though your heart is “skipping” beats or not beating as often as it should.
Other symptoms include:
- Fatigue
- Dizziness
- Lightheadedness
- Sweating
- Fainting
- Shortness of breath
- Chest pain
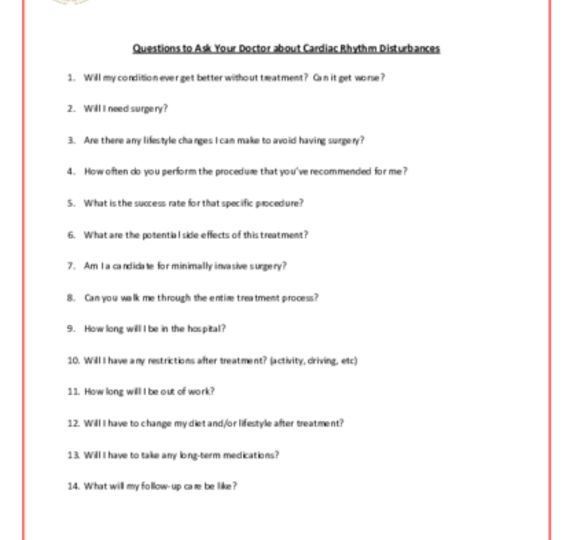
Your doctor usually can diagnose a cardiac rhythm disturbance based on your symptoms, medical history, risk factors, a physical exam, and with results from tests and procedures.
During a physical examination, your doctor will check your heart rate and rhythm, together with your pulse. If your doctor believes you may have a cardiac rhythm disturbance, he or she likely will order an electrocardiogram (EKG) for confirmation.
There also is a more advanced version of an EKG where your doctor may ask you to wear an “event” (or “Holter”) monitor. This is a portable device that is the size of a smartphone or smaller and can be worn under clothing, similar to an exercise heart rate monitor. This device will relay information back to your doctor and identify any abnormal rhythms that might happen intermittently, but not all of the time. The monitor usually is worn for 24-48 hours to get the required information.
Your doctor also may recommend one or more of the following: echocardiogram (echo), chest x-ray, blood tests, stress test, and coronary angiography. For more information on these tests, visit our common diagnostic tests page. If your family doctor discovers the heart rhythm problem, you likely will be referred to a cardiologist (general heart specialist) or an electrophysiologist (heart rhythm specialist).
Together with you and your medical team, your doctor will determine the best treatment option based on your symptoms and test results.
As a first step, your doctor likely will try to treat your cardiac rhythm disturbance with medications that help restore your heartbeat to a normal rhythm. In some circumstances, that medication regimen may also include blood thinners to prevent blood clots from forming in your heart. It is important to take these medications exactly as directed to reduce the chance of side effects.
As a first step, your doctor likely will try to treat your cardiac rhythm disturbance with medications that help restore your heartbeat to a normal rhythm. In some circumstances, that medication regimen may also include blood thinners to prevent blood clots from forming in your heart. It is important to take these medications exactly as directed to reduce the chance of side effects.
Additionally, it's possible that your doctor may try to “shock” your heart out of the abnormal rhythm. This is called a cardioversion, and it is a procedure where medication would be given to make you drowsy so that you would experience no pain or awareness during the short procedure.
Additionally, it's possible that your doctor may try to “shock” your heart out of the abnormal rhythm. This is called a cardioversion, and it is a procedure where medication would be given to make you drowsy so that you would experience no pain or awareness during the short procedure.
If medications or cardioversion cannot maintain a normal heart rhythm, your doctor may recommend a treatment such as a pacemaker, an ablation, or a combination of therapies. An ablation is when an electrophysiologist attempts to disrupt, or ablate, the abnormal electrical signals and allow your heart to use the normal pathways instead. This procedure can take several hours but is performed through a blood vessel in the groin with special instruments and devices and does not require heart surgery.
When these less invasive methods are not working, or if your doctors feel like your heart might not respond to them, surgery may be recommended. Your doctor can refer you to a cardiothoracic surgeon, who can review all surgical treatment options with you.
If medications or cardioversion cannot maintain a normal heart rhythm, your doctor may recommend a treatment such as a pacemaker, an ablation, or a combination of therapies. An ablation is when an electrophysiologist attempts to disrupt, or ablate, the abnormal electrical signals and allow your heart to use the normal pathways instead. This procedure can take several hours but is performed through a blood vessel in the groin with special instruments and devices and does not require heart surgery.
When these less invasive methods are not working, or if your doctors feel like your heart might not respond to them, surgery may be recommended. Your doctor can refer you to a cardiothoracic surgeon, who can review all surgical treatment options with you.
Surgery for atrial rhythm problems is called the Maze Procedure. This is similar to the ablation, but uses different ways to disrupt the abnormal electrical channels. One way is to cut them, freeze them, or even make small burns to create scars over the abnormal areas so that the heart will use the normal electrical pathways instead. Doing this requires direct vision of the heart, and therefore a surgical incision is made on the chest cavity. Sometimes cameras are used to allow smaller incisions, but your surgeon will discuss the safest and most appropriate approach for you.
In patients who have atrial fibrillation in addition to other forms of heart disease, the Maze procedure is frequently performed along with other open heart surgical procedures, such as mitral valve repair or replacement.
Surgery for atrial rhythm problems is called the Maze Procedure. This is similar to the ablation, but uses different ways to disrupt the abnormal electrical channels. One way is to cut them, freeze them, or even make small burns to create scars over the abnormal areas so that the heart will use the normal electrical pathways instead. Doing this requires direct vision of the heart, and therefore a surgical incision is made on the chest cavity. Sometimes cameras are used to allow smaller incisions, but your surgeon will discuss the safest and most appropriate approach for you.
In patients who have atrial fibrillation in addition to other forms of heart disease, the Maze procedure is frequently performed along with other open heart surgical procedures, such as mitral valve repair or replacement.
If you require surgical treatment for your cardiac rhythm disturbance, you should expect to be in the hospital for about a week after surgery. Your hospital stay likely will include a day or two in the intensive care unit (ICU) where hospital staff can monitor your blood pressure, breathing, and other vital signs. You also will have a breathing tube for a few hours or possibly overnight, so communication will be difficult. The breathing tube will be removed as soon as you are awake and able to breathe on your own.
Most patients can be discharged from the hospital within a week, but recovery continues at home. This is an individual process that is affected by your age and general health status, but most patients initially need to modify some activities and require a few weeks to re-gain energy levels.
Often a period of “cardiac rehab” or working out at a designated gym a few times a week for reconditioning is recommended.
Many patients can return to work within 4-6 weeks, but this depends on the type of job and general recovery progress. Your doctor will provide individualized recommendations for your full recovery.
Adopting a healthy lifestyle also will help manage your risk factors for developing another cardiac rhythm disturbance. This can include:
- Eating a heart-healthy diet
- Getting and staying active
- Reducing high blood pressure
- Lowering and controlling your cholesterol levels
- Losing any excess weight
- Quitting smoking
Reviewed by: Robbin G. Cohen, MD, with assistance from John Hallsten and Travis Schwartz
July 2016
Previously reviewed by: Emily A. Farkas, MD