Tetralogy of Fallot
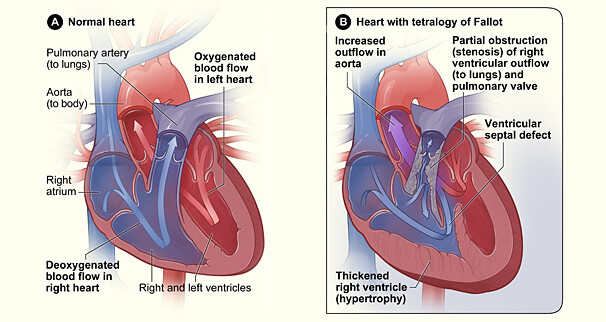
Tetralogy of Fallot (te-tral-uh-jee; fa-loh) is a rare, complex series of four congenital (present at birth) heart defects that occur while your baby is still growing inside the womb.
According to the American Heart Association, congenital heart defects (present at birth) are the most common type of birth defect. They affect 8 out of every 1,000 newborns. Each year, more than 35,000 babies in the United States are born with congenital heart defects.
Although the condition is rare, Tetralogy of Fallot (TOF) is the most common congenital (present at birth) heart defect causing a “blue baby.” According to the National Heart, Lung, and Blood Institute (NHLBI), TOF affects roughly 5 out of every 10,000 babies. The defect is found equally among boys and girls.
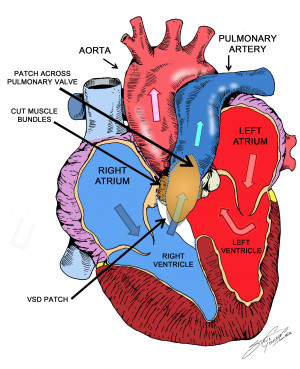
The only treatment for tetralogy of Fallot is open heart surgery.
Babies who have surgery to repair TOF usually do well. More than 90% survive to adulthood and live active, healthy, and productive lives.