- Adult Heart DiseaseDiseases of the arteries, valves, and aorta, as well as cardiac rhythm disturbances
- Pediatric and Congenital Heart DiseaseHeart abnormalities that are present at birth in children, as well as in adults
- Lung, Esophageal, and Other Chest DiseasesDiseases of the lung, esophagus, and chest wall
- ProceduresCommon surgical procedures of the heart, lungs, and esophagus
- Before, During, and After SurgeryHow to prepare for and recover from your surgery
May 21, 2018

Once you and your doctor have decided that surgery will be a part of your treatment plan for lung cancer, it’s a good idea to prepare yourself for things to come. This article will guide you in thinking about more detailed questions to ask your surgeon and care team.
Common concerns
How long will my recovery be?
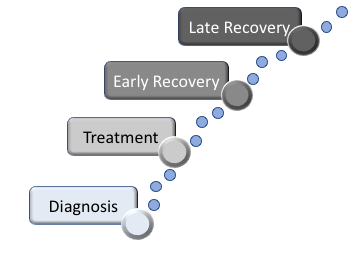
Time for full recovery after surgery largely depends on two factors:
- The type of surgery you have
- Your level of conditioning and function prior to surgery
Recovery from lung cancer surgery can vary significantly from a couple of weeks to several months. Traditional lung operations are performed through a thoracotomy (a long incision on the side of the chest), which involves spreading the ribs. These surgeries, which can be necessary for large tumors or very complex surgical resections, can be associated with longer recoveries.
Increasingly more common is the use of newer minimally invasive surgical techniques (video-assisted thoracoscopic surgery or VATS) which are performed by experienced thoracic surgeons and do not involve spreading of the ribs. Patients who are able to have VATS instead of a thoracotomy tend to have less pain after surgery and recover more quickly.
If your lungs are in good condition and your activities of daily living are not otherwise limited, you should expect to return to your normal level of activity following the surgical recovery. Given the linkage of smoking and lung cancer, it is not uncommon for patients with lung cancer to also have some degree of lung disease, such as emphysema, which can be made worse after surgery. Your doctor should be able to review this risk with you based on the breathing tests done prior to surgery. It is important to maintain good baseline level of daily activity in the days leading up to surgery which will be helpful for your recovery both in the hospital and once you return home.
Will I need assistance when I go home from the hospital?
You will be able to provide routine self-care including bathing and dressing by the time you are discharged from the hospital. Many people still find it helpful to have a friend or family member available to provide assistance if necessary and check on you once you return home. You may find that you have a reduced appetite. However, it is important to maintain a healthy diet to aid in healing and recovery. Try to eat small regular meals and avoid alcohol consumption, especially while taking prescription pain medication.
If I’ve had chemotherapy or radiation therapy, does that make my surgery different in any way?
Your therapy might including a combination of surgery with chemotherapy and/or radiation therapy. It’s important to know that radiation therapy has the potential to make surgery more difficult due to scar tissue that forms in your chest. Because of this, make sure your surgeon has sufficient experience in treating patients under these circumstances.
How will surgery affect my breathing?
It is normal to experience some degree of shortness of breath after all surgeries and that certainly is the case after surgery to remove a portion of the lung. The degree of breathlessness you experience is dependent on a host of factors, including:
- Type of surgery
- Amount of lung function you have prior to surgery
- Other medical conditions you may have (such as heart disease)
- Any complications you may have experienced after surgery
In general, you might experience mild breathlessness when transitioning home and while doing things such as getting dressed, showering, or going up stairs. This normally improves quickly with a short rest and continues to improve as your remaining lung adapts, pain subsides, and you regain your stamina.
Prior to surgery, most patients are instructed on the use of an incentive spirometer, which is used for patients undergoing lung surgery. This small handheld device helps you to expand your lungs by performing deep breathing exercises in a precise way. It provides measurable feedback on how well you are filling your lungs with air as you inhale deeply.

Early Recovery and Transitioning Home
Wound care and bathing
By the time you are discharged from the hospital, you should no longer have bandages on your wounds. If you do, your surgical team will have provided you with special wound care instructions. Under most circumstances, the wound is left open to air. Avoid using any lotions, creams, powders, or ointments unless specifically instructed by your surgical team, as these may cause infection or skin problems. You may have a suture remaining from your chest tube, which will be removed at your postoperative visit. You may shower with warm water as soon as you are discharged from the hospital. It is okay to wash the incision gently with mild soap and without rubbing. Your doctor may recommend that you not take a tub bath or use a Jacuzzi for approximately 4 weeks.
It is important to monitor your wound daily for signs of infection. Using a mirror can help. You will be given specific instructions at the time of discharge with telephone numbers to call with concerns. Notify your care team if you experience any of the following:
- Increased drainage
- Swelling or oozing from the incision
- Opening of the incision line
- Redness around the incision
- Warmth along the incision line
- Increased body temperature (greater than 101°F or 38°C)
Follow-up visits
You can expect to have at least one follow-up visit with your surgeon to check on your progress and recovery. This is usually 2 weeks after discharge. In addition, you may receive a phone call from the doctor’s office or the hospital within 48 hours of returning home.
At the first follow-up visit, you can expect to have any remaining sutures or staples removed, address any specific concerns, review your pathology report, and outline next steps for follow-up and care. A chest x-ray is frequently taken at the initial postoperative visit.
Pain and medications
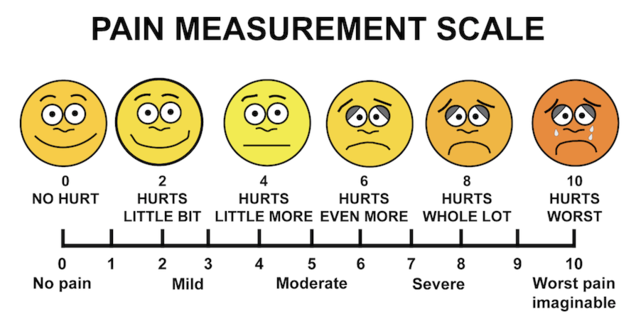
The most common symptoms patients are experiencing at the time of the first postoperative visit are:
- Pain
- Dry cough
- Easy fatigability
- Breathlessness
Pain may still be present but is usually minimal by this time, particularly if a VATS procedure was performed. Prescription pain medications can be weaned and non-steroidal medications can help in this transition. Pain management is important to help you return to normal physical activity faster and avoid complications such as pneumonia and blood clots.
Numbness of Incision Area
Nearly all patients will report temporary numbness around the incision area(s). This is due to manipulation of the nerves that are located between the ribs during surgery. It may take several months for this to improve, although it may never resolve completely.
Constipation
Constipation is common, especially with pain medications. Make sure to keep mobile and drink plenty of fluids. Eating fruits and vegetables also will help combat constipation. You also may be given stool softeners at the time of discharge.
Reviewing your pathology report
The final pathology report may take 1-2 weeks to complete. Your doctor will review it with you at the time of your follow-up visit. The main components of the report include confirmation of what type of tumor was present and whether the entire tumor was removed. Another important factor is whether the tumor has spread to other structures, including lymph nodes. This information, along with other preoperative test results, will help your doctor establish your final cancer stage. The cancer stage will determine whether additional therapy is recommended.
Late Recovery
Depending on your recovery, your doctor may request another short-interval visit before transitioning you to long-term follow-up. Any lingering concerns not previously addressed can be discussed at this visit and often include conversations regarding:
Return to work
The routine timeline of weeks to months can change depending on your occupation and/or eagerness to return to normal activity. Financial concerns, driving and transportation concerns, and pain levels also are taken into consideration. Since prescription pain killers can impair reflexes, driving should be avoided while still taking them. In general, you will work with your provider to determine the best time for you to return to work.
Chronic pain
A small proportion of people may find that they have pain that lasts for a long time after surgery. This type of chronic pain, known as Post-Thoracotomy Pain Syndrome, is rare, affecting approximately 1%-10% of people following chest surgery. The pain is from nerves that run along the operation scar between the ribs which can be damaged during the operation. In these cases, the pain gradually reduces over time, but can take up to a couple of years as the nerves attempt to repair themselves. For some people, it may continue for longer. This type of nerve pain can be difficult to control with traditional pain medication and patients often must see a pain specialist for help.
Survivorship/Emotional wellbeing
Any major surgery can make a patient sad or depressed after leaving the hospital. Added to this can be the emotions associated with a new diagnosis of lung cancer. Patients may feel anxiety about the future or may be more emotional from being extra tired or irritable because of the surgery itself and post-operative medications. These feelings are usually temporary and should go away as you resume your normal routine activities.
Sometimes, patients may feel a strong sense of sadness or depression that persists for more than a couple of weeks and prevents them from returning to normal activity. If this happens, you should talk to your doctor or a mental health specialist. There are many resources to help patients cope with the emotions surrounding cancer and recovery from surgery, including support groups, one-on-one counseling, and medications. All of these options will help you feel better, enhance your recovery, and return you to normal activity sooner.
Read more about Lung Cancer.
The opinions expressed in this article are those of the author and do not necessarily reflect the views of The Society of Thoracic Surgeons.

